Current Pediatric Research
International Journal of Pediatrics
Epidemiological trends, clinical presentation, management and outcomes of acute respiratory infections in children admitted to Kara teaching hospital.
Segbedji KAR1, Tchagbele OB1*, Talboussouma SM1, Takassi OE2, Agrigna H2, Sadio Tiokang AJ2, Atakouma YD2, Azoumah KD1
1Department of Epidemiology, University of Kara, Kara, Togo
2Department of Epidemiology, University of Lome, Kara, Togo
- Corresponding Author:
- Dr. Tchagbele Ouro-Bagna
Department of Epidemiology,
University of Kara,
Kara,
Togo
E-mail: otchagbele@gmail.com
Received: 24 June, 2019, Manuscript No. AAJCP-24-14089; Editor assigned: 29 June, 2019, Pre QC No. AAJCP-24-14089 (PQ); Reviewed: 13 July, 2019, QC No. AAJCP-24-14089; Revised: 01 September, 2024, Manuscript No. AAJCP-24-14089 (R); Published: 29 September, 2024, DOI: 10.35841/0971-9032.28.09.2346-2350.
Introduction: According to Word Health Organization (WHO) in 2015, Acute Respiratory Infections (ARI) are responsible for around three (03) million deaths per year in developing countries. The main of this study was to describe the epidemiological, clinical, therapeutic and outcome of ARI in children at Kara teaching hospital. Methodology: This was a descriptive study on the medical records of children from 1 month to 15 years hospitalized in pediatric unit from January 1, 2015 to December 31, 2016. The main parameters studied were the medical history of allergy, the season, the clinical and radiological signs, the treatment and outcome. Results: ARI accounted for 8% of hospitalizations, mainly affected the children under 5 years of age (81%) specially the infants (54.6%). The sex ratio was 1.62. The reasons for consultation were dominated by cough (84.6%), fever (81.7%) and breathing difficulties (34.8%). Tachypnea (57.1%), bronchial groans (52.4%), signs of struggle (35.9%) and crackling groans (34.4%) were the dominant clinical respiratory signs. According to the classification of Integrated Management of Childhood Illness (IMCI), there was severe pneumonia in 37.4%, pneumonia in 40.3%. The chest x-ray (47.6%) showed flaky (46.1%) and linear (38.5%) opacities. The main topographic forms were bronchopneumonia (51.3%), rhinobronchitis (26.4%) and bronchitis (13.6%). The co-morbidities were undernutrition (9.9%) and HIV infection (8.8%). Antibiotic therapy was used in 96.3% of cases. The average hospital stay was 4.6 days. The lethality was 5.5%. Conclusion: The morbidity and mortality linked to ARI remains high. The efforts remain to be made for prevention and early management of cases.
Keywords
Acute respiratory infections, Epidemiology, Child, Mortality, Togo.
Introduction
Acute Respiratory Infections (ARI), especially pneumonia, are responsible for around three (03) million deaths a year in children under age of 5 years in developing countries. The ARI therefore represent a significant burden of mortality in children under 5 years. Despite the various health policies implemented to improve child survival, the morbidity and mortality linked to ARI remain high in developing countries, especially in Togo where in 2013, the prevalence of ARI was estimated at 7%.
In Togo, there have been several studies either on upper ARI or lower ARI. However, the only work on upper and lower ARI backed to 2010 and concerned only children under 5 years. It therefore appeared necessary to conduct this study including all children in order to determine the part of ARI in children’s illnesses and appreciate the different aspects in a hospital ward. It was in this context this work was done at teaching hospital of Kara (in northern Togo). The aim of this work was to describe the epidemiological, clinical, therapeutic and outcome aspects of acute respiratory infections in children hospitalized Kara’s teaching hospital [1].
Materials and Methods
This study was conducted in the pediatrics department of Kara’s Teaching Hospital. This was a retrospective descriptive study during 24 months from January 1st, 2015 to December 31st, 2016. All hospitalized children between one month and 15 years (180 months) and who had respiratory signs related to an ARI (fever with cough or cold or breathing difficulties evolving for less than two weeks) were included. Data collection, by manual examination, was carried out using a survey from the medical records of hospitalized children and the admission and discharge registers of the pediatric unit. The main parameters studied were epidemiological (period of admission, civil status data, comorbidities), clinical (disease’s history, clinical and para clinical data), therapeutic and outcome. The data analysis was done with excel, word and EPI info version (TM) 3.5.1 software. The chi-square test was calculated to compare some variables with a significance level of "p" set at 0.05. Fisher's exact test was used for numbers below 5. The patient’s anonymity was respected throughout the data collection process [2-4].
Results
Out of 3,422 children hospitalized during the study period, 273 cases of ARI were retained, constituting 8% of hospitalizations. The mean age of the children was 32.9 months with extremes of 1 and 180 months. There were 221 (81%) children under the 5 years, 101 (45.7%) of whom were under 12 months of age and 48 (21.7%) between 12 and 24 months of age. Regarding gender, there were 169 boys (62%) and 104 girls (38%). The sex ratio was 1.62 [5-7].
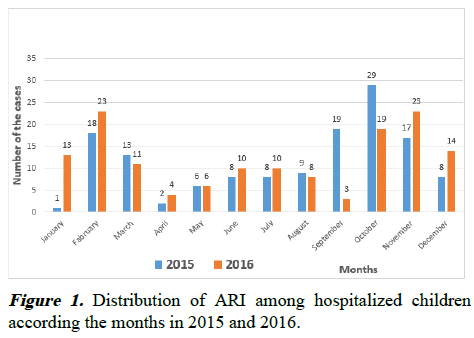
Depending on the period of occurrence, ARI were observed throughout the year with peaks in February, September and October-November (Figure 1).
Clinical aspects
The reasons for consultation were dominated by cough (84.6%), fever (81.7%), breathing difficulties (34.8%), vomiting (31.9%) and rhinorrhea (28, 2%). The main general signs were fever (72.2%), pallor (49.1%), asthenia (37.4%) and dehydration (5.1%). The respiratory signs were: Tachypnea (57.1%), respiratory signs of struggle (35.9%), bronchial groans (52.4%), crackling groans (34.4%), sibilant groans (13.9%), the reduction/abolition of the vesicular whisper (4.0%) and the rattling groans (3.7%). Respiratory distress was observed in 98 cases (35.9%): According to the Silverman score, it was severe (8%), moderate (33%) or mild (59%). The other common physical signs observed were altered consciousness (7.0%) and abdominal bloating (6.6%). The nutritional status was normal in 246 cases (90%). A severe and a moderate acute undernutrition were found in respectively 3.3% and 6.7%.
The chest radiography was performed in 130 children (47.6 %). Abnormal radiographic images were observed in 118 children (90.8%) dominated by flaky and linear opacities in respectively 60 (44.2%) and 50 (38.5%) cases. The complete blood count carried out in 212 cases (77.6%) noticed as main anomalies anemia (88.2%), hyper leukocytosis with neutrophils (17.4%) and lymphocytosis (9%). The sedimentation rate achieved in 30 cases (11%) was accelerated in 26 cases (9.5%). The malaria test performed in 199 febrile children (72.9%) was positive for Plasmodium falciparum for 69 children (25.3%). HIV testing was positive for 25 children (9.2%). Bronchopneumonia (51.3%), acute rhinobronchitis (40.0%), pneumonia (8.8%) and acute bronchiolitis (7.7%) were the main types of ARI. Regardless of the topographic form of ARI, infants (1 to 30 months) were most affected (Table 1) [8].
The assessment of cough and difficulty in breathing according to the IMCI classification noted severe pneumonia and pneumonia respectively in 37.7% and 41% (Table 1).
| Age (month) | Broncho pneumonia | Rhinobronchitis | Pneumonia | Bronchiolitis |
|---|---|---|---|---|
| 1-30 | 81 | 56 | 15 | 21 |
| 30-60 | 28 | 12 | 1 | 0 |
| 60-144 | 25 | 4 | 5 | 0 |
| 144-180 | 6 | 0 | 3 | 0 |
| Total | 140 | 72 | 24 | 21 |
Table 1. Distribution of the main topographical forms of ARI according to the age of children.
The pathologies associated with ARI were malaria (25.3%), acute bacterial gastroenteritis (20.9%), acute undernutrition (severe and moderate) (10%), pediatric AIDS (9.2%), vaso- occlusive crisis of SS sickle cell anemia (1.5%), heart disease (0.7%) and acute meningococcal meningitis (0.4%).
Therapeutic aspects
Among the 273 children hospitalized for ARI, 145 (53.1%) received pre-hospital treatment consisting of antipyretics (30.2%), antimalarial (27.1%), antibiotics (26.5%), corticosteroid (8.8%), antiemetic (7.0%), cough suppressant (4.0%), antihistamine (2.9%), thinning agent (2.6%), bronchodilator (1.8%), nasal decongestant (0.4%) and traditional remedy (1.5%). The main antibiotics used before hospitalization were penicillin A (13.6%), third generation cephalosporins (9.2%), macrolides (3.7%). Inpatient treatment was based on antibiotics (96.3%): Third generation cephalosporins associated with aminoglycosides (64.5%), penicillin A (27.8%), macrolides (16.1%), antimalarial (73.3%), antipyretic (58.2%), corticosteroid (24.2%), bronchodilator (11.4%) and mucolytic (3.7%). Adjuvant therapy was based on blood transfusion (10.3%), nasopharyngeal clearing with physiological water (9.5%) and oxygen therapy (5.9%) [9].
Outcome
The hospital stay varied from 1 to 29 days with an average of 4.60 days. The hospital stay was variable: 1 to 2 days (16.1%), 3 to 7 days (72.5%), 8 to 14 days (9.5%) and 14 days and more (1.8%). The outcome was favorable (cure) in 70, 7% of the cases. The death rate was 5.5% (15 cases). The 15 cases of death mainly concerned infants under 24 months (9/15 cases). Death was mainly linked to bronchopneumonia or severe pneumonia according to IMCI (12/15 cases) with a p equal to 0.0005. An exit against medical advice was noted in 19.8% of cases and an escape in 4% of the cases.
Discussion
This work evaluated ARI in hospitalized children. It emerges from this work that ARI represented 8% of hospitalizations at Kara’s teaching hospital. The peak frequency of ARI was recorded in February, September, October and November. Children under 5 years are the most affected in 81% among which 67.5% were less than 24 months old. In just over a third of the cases (35.9%), these children arrived at the hospital in a respiratory distress warranting urgent care. According of the topography, it was most often bronchopneumonia (51.3%), acute rhinobronchitis (40.0%), pneumonia (8.8%) and acute bronchiolitis (7.7%). The average hospital stay was 4.6 days. Malaria and HIV were associated with ARI in respectively 25.3% and 9.2%. The situation of children under 5 years, especially those under 24 months in terms of ARI remains similar in hospitals in Togo compared to the situation which prevailed in 2005 where 79.8% of children under 24 months were affected by ARI at CHU-Tokoin [10].
Epidemiological aspects
Acute respiratory infections are the leading cause of death and morbidity in children under 5 years of age behind neonatal causes. This result is similar to that recorded in Senegal where children under 5 years represent 85% of those hospitalized for ARI in the pediatric service. Therefore, ARI remains a major public health problem especially in developing countries. An alternative policy in the reduction of morbidity and mortality linked to a policy focused on improving community management of ARI at the onset of symptoms and rapid access to care, especially for parents with low or average incomes will be an alternative policy in the reduction of morbidity and mortality linked to ARI. The sex ratio was 1.62. This male predominance has also been described in Senegal in two studies. In India, boys have 2.4-fold higher hospitalization’s rate than girls about ARI. We do not have an explanation for this finding.
ARI accounted for 8% of hospitalizations. This frequency was 3.7% in the study of Diagne, et al. Although hospital frequency varies from one center to another or one country to another, the reality of morbidity and mortality from ARI remains the same in developing countries due to its impact on the health of children under the age of 5 years [11].
Diagnostic aspects
Cough is a reflex phenomenon with a bronchopulmonary starting point which aims to protect the airways from foreign particles or to eliminate the particles produced. It is therefore the most frequent reason for consultation encountered in consultation for ARI. Indeed, coughing was the most frequent sign (84.6% of cases) in our work. The cough is almost always accompanied by fever, found in 81.7% of the reasons for consultation in our series. As in our work, in the series of Diagne, et al., fever and cough were found in the same proportions where it represented 94.5% of the reasons for consultation. A febrile cough should lead to a search for an ARI because of the morbidity and mortality due to ARI in developing countries. In anyway, a cough, whether febrile or not, should lead to an exploration of the respiratory tract to avoid secondary aggravations which are sources of hospitalization and costs which weaken the socioeconomic situation of parents already precarious in our countries. Respiratory distress accompanied cough in 34.8% of cases. This result is close to that of Kemp and Shelton, who reported 33% of cases of ARI with dyspnea and that of Guittet, et al., with 28.9% of dyspnea. Bach, et al., on the other hand, found a higher rate with 57.7% being asked the authors if viral infections might not be more likely to trigger episodes of dyspnea. Diagne, et al, found respiratory distress in 6.4% of the cases but yet 82.6% and 80.7% of the children had respectively a positive bacteriological and virological sample, so questioning the conclusions of Bach, et al.
Topographically, bronchopneumonia (51.3%), acute rhinobronchitis (40.0%), pneumonia (8.8%) and acute bronchiolitis (7.7%) were the main types of ARI in hospital. These are almost essentially low-grade ARI, the most prevalent of which is bronchopneumonia. Pneumonia and bronchopneumonia were the most prevalent lower ARI in hospitalization in the series of Ly, et al. However, in the study of Sougou in Senegal on ARI in general, bronchiolitis (38.5%) was the first cause of ARI followed by acute tonsillitis (17.3%), bronchopneumonia (17.3%) then pneumonia (13%).
These studies show that lower ARI is the main cause of hospitalization of ARI in children.
A chest x-ray is one of the exams of choice for diagnosing lower ARI. Although, sometimes the expression of radiological signs is offset from that of physical signs; of the 130 chest xrays taken, abnormal images were observed in 43.2% of children with a predominantly alveolar syndrome (22.0%). The alveolar syndrome reflects a parenchymal attack (pneumonia). This result can therefore be explained by a significant frequency of bronchopneumonia in our study. The abnormalities in the hemogram can guide the diagnosis of ARI and identify complications or underlying comorbidities such as anemia found in 88% in our study. The present study allowed us to report hyperleukocytosis with neutrophilic polynucleosis in 17.4% of cases and lymphocytosis in 9% of cases. Hyperleukocytosis is an indicator of infection, when it is predominantly neutrophil it evokes a bacterial etiology and when it is lymphocytic it evokes a viral etiology. This result therefore advances a predominance of bacterial infection in our study. The absence of an abnormality of the white blood line at the complete blood count in the rest of the children could be explained by the untimely antibiotic therapies often by selfmedication which was the subject of some children before their admission. In fact, 26.5% of the children admitted had already used an antibiotic [12].
Infants under 30 months of age were the most affected whatever the topographical form of ARI, with in particular 17 cases of bronchiolitis out of the 21 cases (81%) and 81 cases of bronchopneumonia out of the 140 cases (58%). Lower respiratory infections, especially pneumonia, are the main causes of morbidity and mortality in children under 5 years in Africa. The pathologies associated with ARI were anemia (88%) malaria (25.3%), acute bacterial gastroenteritis (20.9%), acute undernutrition (severe and moderate) (10%), pediatric AIDS (9.2%). In Benin, Adedemy, et al., found malaria (85.6%), anemia (78.1%), meningitis (23.2%) and malnutrition (21.9%) as pathologies associated with ARI in children under 5 years. The anemia favored by malnutrition and malaria constitute frequent comorbidities which weaken children under 5 years and worsen ARI making treatment difficult. It should therefore be emphasized that malnutrition creates a vicious circle with ARI, as found by Ngombe, et al., where 41.2% of children under 5 years hospitalized for ARI were undernourished.
Therapeutic aspects
It is common in our hospitals to receive children after a first attempt to treat their illnesses either by parental self-medication or by using a first level of care. In our series, 53.1% of patients had received treatment with antipyretics (57.9%), anti-malarials (51%), antibiotics (26.5%) before hospitalization.
Asseray, et al., in France in 2013 reported 63.7% selfmedication in the 2 weeks preceding a consultation. This rate is higher than that we found. The reasons for such high selfmedication in the context of Asseray, et al., study could be explained by the impression that the pathological situation is a secondary importance, the feeling of having already experienced a comparable symptomatology that we know how to treat and the fear of learning that It is a serious illness. Group A penicillins were the most used antibiotics before hospitalization in our study representing 50% of the antibiotics used. This rate can be explained by the easily manipulable nature of group A penicillins and over-the-counter sales even in pharmacies; which makes the drugs very accessible thus explaining delays in diagnosis and atypical clinical pictures. Due to the difficult to identify the responsible germ of ARI, the treatment of ARI is often probabilistic according to the anatomo-clinical forms and the suspected germs. In our study, 96.3% of patients received antibiotics during their hospitalization. This high rate of antibiotic use could be justified by the seriousness of signs on admission but also by the fact that 26.5% of patients had already started a previous antibiotic-based treatment. It was therefore necessary to continue antibiotic therapy until there was proof of the absence of a bacterial infection often difficult in our context. According to Gendrel, the clinical difficulty in differentiating a bacterial from a viral etiology or the bacterial overestimation in the event of respiratory infection underlies this systematic use of antibiotics.
Outcome
The average of hospital stay in our series was 4.60 days. Diagne, et al., found an average hospital stay of 10 days. The bacteriological and virological examinations carried out in their work could explain this long duration of hospitalization. Indeed, it was necessary to wait for the results of bacteriology most often before adapting the antibiotic and deciding on the release of the children and it could take a few days. The letality rate for ARI in our study was 5.5%. The death was mainly linked to bronchopneumonia (12 cases out of 15). This finding confirms that pneumonia or bronchopneumonia remains a fatal respiratory infection. The delay in consultation due to selfmedication is an undeniable element in the occurrence of deaths as noted by Diagne, et al., in Senegal.
Conclusion
This study evaluated the ARI found in hospitalization in children at CHU Kara. It appears that bronchopneumonia is the most common and most lethal ARI. The main associated comorbidities were anemia, malaria, acute bacterial gastroenteritis, acute undernutrition (severe and moderate) and pediatric AIDS.
Conflict of Interest
None.
References
- Ferkol T, Schraufnagel D. The global burden of respiratory disease. Ann Am Thorac Soc 2014; 11: 404-406.
[Crossref] [Google Scholar] [PubMed]
- Douti NK, Balaka B, Dassa KS, et al. Acute upper respiratory infections in infants and children: Epidemiology and clinical manifestations. J Rech Sci Univ Lome 2012;14ss:139-142.
- Bakonde B, Tatagan K, Kessie K, et al. Hospital epidemiology of Acute Lower Respiratory Infections (ARI) in Togolese infants and children. Black Afr Med 1998; 45: 435-439.
- Agbere AD, Agbobli E, Assimadi JK, et al. Clinical, therapeutic and evolutionary aspects of pleuropulmonary staphylococcal disease in infants at the Lome-Tokoin University Hospital (Togo). Med Afr Noire 1995: 260-266.
- Guedehoussou T, Atakouma Y, Gbadoe AD, et al. Evaluation of the management of acute respiratory infections in children under 5 years of age at the Lome University Hospital (Togo). J Rech Sci Univ Lome 2010; 12.
- Sougou NM. Epidemiological aspects of acute respiratory infections in pediatric hospitals in Dakar, Senegal. Afr Malag J Sci Res Heal Sci 2019; 1.
- Rasmussen Z, Pio A, Enarson P. Case management of childhood pneumonia in developing countries: Recent relevant research and current initiatives. The Int J Tuberc Lung Dis 2000; 4: 807-826.
[Google Scholar] [PubMed]
- Krishnan A, Amarchand R, Gupta V, et al. Epidemiology of acute respiratory infections in children-preliminary results of a cohort in a rural north Indian community. BMC Infect Dis 2015; 15: 1-10.
[Crossref] [Google Scholar] [PubMed]
- Fuller RW, Jackson DM. Physiology and treatment of cough. Thorax 1990; 45: 425.
[Crossref] [Google Scholar] [PubMed]
- Guittet V, Brouard J, Vabret A, et al. Rhinovirus and acute respiratory infections in hospitalized children. Retrospective study from 1998 to 2000. Arch Pediatr 2003;10: 417-423.
- Bach N, Cuvillon D, Brouard J, et al. Acute respiratory infections due to human metapneumovirus in children: Descriptive and comparative studies with respiratory syncytial virus. Arch Pediatr 2004; 11: 212-215.
- Issoufou MG. Epidemiological, diagnostic, therapeutic aspects and short-term prognosis of acute lower respiratory infections in children at the Niamey Regional Hospital. Malian J Infectiol Microbiol 2024; 19: 48-53.