Current Pediatric Research
International Journal of Pediatrics
Short stature in transfusion dependant beta thalassemia children.
Jagroop Singh Sangha1, Prabhpreet Kaur Sira2*
1Department of Pediatrics, Government Medical College, Amritsar, Punjab, India
2Department of NNF Fellow, Fortis Hospital, Shalimar Bagh, New Delhi, India
Corresponding Author:
- Prabhpreet Kaur Sira
Department of NNF Fellow Fortis Hospital
Shalimar Bagh
New Delhi
India
E-mail: preetsira@gmail.com
Accepted date: August 15th, 2021
Background: Due to high prevalence of beta thalassemia in North India, we conduct this study to assess the prevalence of short stature in such cases. Objective: Study the prevalence of short stature in transfusion dependant beta thalassemia in children aged 5 years-18 years and its correlation with transfusion frequency. Materials and Methods: This is a cross sectional study performed at pediatrics department, government medical college, and Patiala included 93 cases of transfusion dependant beta thalassemia. Anthropometric data was recorded and height of every child was plotted on Indian academy of pediatrics 2015 growth charts. Short stature defined as height less than 3rd percentile. Data were collected, managed, edited, entered, and analyzed by Statistical Package of Social Sciences (SPSS) software. Receiver operating curve was analyzed for frequency of transfusion and short stature. The level of significance taken for the entire statistical test was a P-value of <0.05. Results: 64 males and 29 females were included aged 5 years-18 years with mean age of 10.09 ± 3.4 years. 41 (44.1%) cases were short stature, including 33 (80.5%) males and 8 (19.5%) females. Mean age of short stature cases was 11.9 ± 2.9 years compared to 8.6 ± 3.1 years in cases with normal height (p-value<0.05). ROC curve between short stature and transfusion frequency showed cut off of 16 days. We observed a significant correlation between frequency of transfusion and the incidence of short stature (P=0.001). Conclusion: Short stature is highly prevalent among multi-transfused beta thalassemia children and hence it is recommended that every patient should be sort out for short stature.
Keywords
H emoglobin, Short stature, Tranfusion
Introduction
The inherited disorders of haemoglobin include the thalassemias and structural variants of haemoglobin. These are the commonest single gene disorders globally with an autosomal recessive inheritance and it is estimated that around 300,000 to 400,000 babies with a severe haemoglobin disorder are born each year. The average prevalence of β thalassemia carriers is 3%-4% which translates to 35 to 45 million carriers in our multi-ethnic and culturally and linguistically diverse population of 1.21 billion people which also includes around 8% of tribal groups according to the census of India 2011 [1].
The recommended treatment for beta-thalassemia major involves regular red blood cell transfusions throughout life, usually administered every two to five weeks depending on the transfusion needs of each individual in order to maintain the pre-transfusion level of haemoglobin between 9 and 10.5 g/Dl [2]. Chronic transfusion therapy dramatically improves the quality and reduces the complications of severe thalassemia; however, transfusion-induced hemosiderosis becomes the major clinical complication of transfusion-dependent thalassemia [3]. Progressive iron deposition in tissues as a result of repeated blood transfusions and enhanced dietary absorption of iron due to ineffective erythropoiesis leads to many complications that may emerge as these children grow into adolescence and adulthood.
The deleterious effects of excessive iron deposition are primarily observed in the heart, liver and endocrine organs like pituitary-gonadal axis, GH-IGF axis, thyroid, parathyroid, pancreas and adrenals. Thus, in this era, the endocrine complications have emerged as an important cause of morbidity and an important determinant of quality of life in children with thalassemia major. The predominant clinical phenotypes include short stature, delayed/arrested puberty, abnormal bone mineralisation, impaired glucose tolerance, hypothyroidism and hypoparathyroidism [4]. In this study, we aim to estimate the prevalence of short stature in patients of transfusion dependant thalassemia in children aged 5 years-18 years.
Subjects and Methods
The present study is a type of cross sectional study and was conducted on 93 transfusion dependants beta thalassemia major children enrolled at thalassemia unit, department of pediatrics and analysis was done in the department of biochemistry, govt. medical college, Patiala, Punjab.
Inclusion criteria
The inclusion criteria were children aged 5-18 years, diagnosed with thalassemia on the basis of haemoglobin electrophoresis or high-performance liquid chromatography and receiving blood transfusion regularly.
Exclusion criteria
Patients with congenital disease and chronic illness other than thalassemia (such as malignancy, tuberculosis, chronic hepatitis, congenital heart disease, chronic renal failure, epilepsy, and diabetes mellitus).
Methods
Patients were verified for fulfilling inclusion criteria and ruled out for presence of exclusion criteria. Informed consent was taken from family members after briefing them about the study in their vernacular language. A detailed history, clinical examination and laboratory workup was done as per the proforma.
Height measurement
Height was measured standing upright after ensuring the height board was on level ground. Shoes, socks and hair ornaments were removed. The back of the head, shoulder blades, buttocks, calves, and heels were all touching the vertical board. The trunk was balanced over the waist, i.e., not leaning back or forward. Child’s head was positioned so that a horizontal line from the ear canal to the lower border of the eye socket runs parallel to the baseboard. Still keeping the head in position, other hand was used to pull down the headboard to rest firmly on top of the head and compress the hair. The measurement was read and child’s height was recorded in centimeters.
Specimen collection
Blood samples, 5 ml each, under all aseptic precautions was conducted by venipuncture and allowed to clot. The serum was then separated by ultracentrifugation of samples at room temp and serum ferritin was performed the same day of collection of sample. Samples were collected in plain vials. Results were entered in the proforma and the height of every child was plotted on IAP 2015 growth charts. Short stature was defined as height less than 3%.
Data were collected, managed, edited, entered, and analyzed by SPSS software. Short stature was computed as per different study characteristics. Receiver operating curve was analyzed for frequency of transfusion and short stature. The level of significance taken for the entire statistical test was a Pvalue< 0.05.
Results
In total, 93 children of transfusion dependant thalassemia were enrolled in the study, which included 64 males and 29 females. The cases belonged to the age group of 5 years-18 years with mean age being 10.09±3.4 years. 44 cases were residing in rural areas and the rest in urban areas. Cases were also categorized according to the Kuppuswamy scale-4 cases belonged to Class-I, 64 in Class-II, 20 cases in class III and 5 cases in Class-IV. No case belonged to Class-V in our study. 48 cases had splenomegaly, 50 had hepatomegaly and 21 cases had both hepatosplenomegaly.
When we assessed the growth pattern of these children, 41 (44.1%) cases were found to have height less than 3rd centile on the growth chart and 52 (55.9%) were of normal height. Out of 41 cases of short stature, 33 (80.5%) were males and 8 (19.5%) were females. Mean age of cases with short stature was 11.9 ± 2.9 years and it was 8.6 ± 3.1 years in cases with normal height (p-value<0.05). The height of patients ranged from 71 cm to 160 cm with mean height of 126.25 ± 14.22 cm. The serum ferritin level, haemoglobin level before transfusion, and transfusion frequency were evaluated in these children. The study revealed mean serum ferritin level was 3233.90 μg/L, 53.66% have serum ferritin level >2,500 μg/L, 48.8% had haemoglobin level of 5-8 g/dL before transfusion, and 58.5% have transfusion frequency twice a month (Tables 1-4).
| Short stature (n-41) | Normal Stature (n-52) | p-value | |
|---|---|---|---|
| Sex | 0.001 | ||
| Male | 33 | 21 | |
| Female | 8 | 31 | |
| Age | 0.01 | ||
| 5-9 years | 9 | 33 | |
| 10-14 years | 24 | 15 | |
| 15-18 years | 8 | 4 | |
| Splenomegaly | 0.161 | ||
| Yes | 22 | 26 | |
| No | 19 | 26 | |
| Hepatomegaly | 0.689 | ||
| Yes | 23 | 27 | |
| No | 18 | 25 | |
| Transfusion frequency | 0.029 | ||
| 11-15 days | 24 | 11 | |
| 16-20 days | 10 | 13 | |
| 21-25 days | 5 | 18 | |
| 26-30 days | 2 | 10 | |
| Serum ferritin | 0.042 | ||
| <1000 ng/ml | 1 | 0 | |
| 1000-2500 ng/ml | 18 | 18 | |
| >2500 ng/ml | 22 | 34 | |
| PretransfusionHB | 0.364 | ||
| 5-8 g/dl | 20 | 22 | |
| 8-10 g/dl | 18 | 27 | |
| >10 g/dl | 3 | 3 |
Table 1. Short stature based on study characteristic.
| Youden Index J | 0.38 |
|---|---|
| Associated criterion | <16 days |
| Sensitivity | 61.00% |
| Specificity | 76.90% |
Table 2. Incidence of short stature.
| Frequency of transfusion | Short stature | Normal stature | P value |
|---|---|---|---|
| <16 days | 25 | 12 | <0.001 |
| >16 days | 16 | 40 |
Table 3. Analysis between variables and short stature.
| B | SE | 95% CI for EXP (B) | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Frequency of transfusion | 0.001 | 0.052 | 0.157 | 0.319 |
Table 4. Analysis between the variables and short stature (logistic regression).
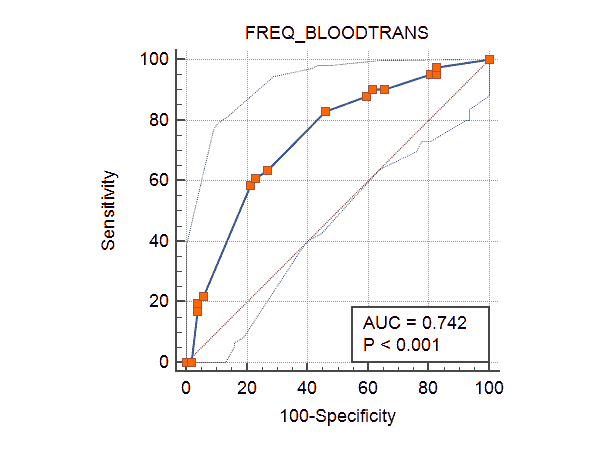
On comparison of short stature with study characteristic like sex, age, average haemoglobin before transfusion, frequency of transfusion, and serum ferritin level, we found a significant correlation between short stature and age, gender, serum ferritin level and frequency of transfusion (P<0.05). Receiver Operating Characteristics (ROC) curve was prepared to evaluate frequency of transfusion cut-off point and short stature incidence. The cut off for transfusion was found to be 16 days with respect to the incidence of short stature (Figure 1).
After obtaining the frequency of transfusion cut-off point, the subjects were divided based on the same. It was analyzed in relation to the incidence of short stature and we observed a significant correlation between frequency of transfusion and the incidence of short stature (P=0.001).
Discussion
Despite major therapeutic progress in the last couple of decades growth failure still is a significant challenge in beta thalassemia major, often affecting the social adjustment and hence quality of life. In the present study, 93 children with transfusion dependant thalassemia were included to study the prevalence of short stature and its correlation with various factors such as age, gender, serum ferritin, pre transfusion haemoglobin and frequency of transfusion. The anthropometric data revealed that short stature was present in 44.1% of the cases included, more common in males (80.5%). The proportion of short stature in our study was comparable to study. Studies by Shamaoon et al. [5,6]. However studies done by Rathaur et al. showed a higher prevalence of short stature [7-9]. This may be attributed to the difference in epidemiological characteristics of the study population included and difference in chelation therapy given to the cases 58.5% of the short statured cases belonged to the age group of 10-14 years with mean age of 10.09 ± 3.44 years (p value<0.05).
Only 7.3% cases of short stature were being transfused adequately as their pre transfusion haemoglobin was more than 10 g/dl, hence suggesting short stature may not only be because of iron overload but other factors like chronic anemia with ineffective erythropoiesis, under nutrition like zinc deficiency, other endocrine dysfunctions and side effects of chelation therapy on skeletal growth also play a role in the growth of the patient 58.5% cases were being transfused atleast twice a month in comparison to 4.9% cases of short stature who were transfused once a month. Hence suggesting higher the volume of transfusion, and hence more iron overload and hence more is the hemosiderosis related injury. Hence, we found a statistically significant correlation between frequency of transfusion and the incidence of short stature (P=0.001). Similar results were obtained in studies by Shamaoon et al. [5,10].
Conclusion
Hence, in conclusion, transfusion dependant thalassemia patients should be adequately transfused so as to prevent development of complications due to the disease. However, iron overload should be prevented and treated with adequate chelation therapy. Regular monitoring of anthropometric parameters on a growth chart at six monthly interval to facilitate early detection of growth faltering.
Transfusion dependant thalassemia patients should be adequately transfused so as to prevent development of complications due to the disease. However, iron overload should be prevented and treated with adequate chelation therapy. Regular monitoring of anthropometric parameters on a growth chart at six monthly interval to facilitate early detection of growth faltering.
References
- Colah R, Italia K, Gorakshakar A. Burden of thalassemia in India: The road map for control. Pediatr Hematol Oncol J 2017; 2(4): 79-84.
- Langhi D, Ubiali EMA, Marques JFC, et al. Guidelines on Beta-thalassemia major–regular blood transfusion therapy: Associação Brasileira de Hematologia, Hemoterapia e Terapia Celular: Project guidelines: Associação Médica Brasileira-2016. Rev Bras Hematol Hemoter 2016; 38(4): 341-5.
- DeBaun MR, Frei-Jones MJ, Vichinsky EP. Thalassemia Syndromes. In: Nelson textbook of pediatrics. Kliegman R, Stanton B, Geme J, Schor N, Behrman R eds. 20th edn. Elsevier Publications. 2016; 2: 2350.
- Singh P, Seth A. Growth and endocrine issues in children with thalassemia. Pediatr Hematol Oncol J 2017; 2(4): 98-106.
- Shamaoon M, Nawaz J, Ahsan M. β-thalassemia major; frequency of short stature in children with β-thalassemia major receiving multiple blood transfusion. Professional Med J 2018; 25(6): 823-7.
- Roth C, Pekrun A, Bartz M, et al. Short stature and failure of pubertal development in thalassaemia major: Evidence for hypothalamic neurosecretory dysfunction of growth hormone secretion and defective pituitary gonadotropin secretion. Eur J Pediatr 1997; 156(10): 777-83.
- Rathaur VK, Imran A, Pathania M. Growth pattern in thalassemic children and their correlation with serum ferritin. J Family Med Prim Care 2020; 9(2): 1166-9.
- Majumdar S, Das PS. A study on growth parameters and clinical profile in children with thalassemia major. IOSR J Dent Med Sci 2019; 18(2): 25-30.
- Fadlyana E, Ma’ani F, Elizabeth M, et al. Correlation between serum ferritin level and growth disorders in children with Thalassemia. Am J Clin Med Res 2017; 5(3): 31-5.
- Aslam MS, Roshan E, Iqbal A, et al. Frequency of short stature in thalassemia major patients. Pak Armed Forces Med J 2013; 63(4): 503-7.