Current Pediatric Research
International Journal of Pediatrics
Herniation of the umbilical cord: A study on clinical spectrum.
Monali Patole, Subhasish Paul*
Department of Paediatrics, Charnock Hospital, West Bengal, India
- Corresponding Author:
- Dr. Subhasish Paul
Department of Paediatrics,
Charnock Hospital,
West Bengal,
India
E-mail: dr.subhasish2017@gmail.com
Received: 19 August, 2019, Manuscript No. AAJCP-24-1322; Editor assigned: 22 August, 2019, Pre QC No. AAJCP-24-1322 (PQ); Reviewed: 05 September, 2019, QC No. AAJCP-24-1322; Revised: 01 August, 2024, Manuscript No. AAJCP-24-1322 (R); Published: 29 August, 2024, DOI: 10.35841/0971-9032.28.08.2313-2315.
Umbilical cord herniation, a rare congenital anomaly, occurs when the small bowel herniates into the proximal umbilical cord, often mistaken as ‘omphalocele minor.’ Mismanagement, such as inadvertent clamping, can lead to bowel injury. This study examines 90 cases of Congenital Umbilical Cord Herniation (CUHC) at a tertiary care government medical college, detailing patient demographics, intraoperative findings, associated malformations and outcomes with a 1-year follow-up. Ileal loops and Meckel's diverticulum were the most common findings. Findings suggest that prompt surgical intervention effectively prevents long-term morbidity and mortality. Additionally, the study discusses embryological factors and emphasizes the importance of early detection through antenatal ultrasound.
Keywords
Congenital herniation, Umbilical cord, Omphalocele, Ileal loops, Meckels diverticulum.
Introduction
Herniation of the umbilical cord is a rare clinical entity which presents with herniation of the small bowel into the proximal part of the umbilical cord. This is sporadically associated with other congenital malformations. This is usually poorly identified and mistakenly termed as ‘omphalocele minor’. Inadvertent clamping of the cord in these cases leads to iatrogenic bowel wall injury. Here we present a series of 90 cases presenting with umbilical cord herniation in a tertiary care Govt medical college, along with demography, intra operative findings, associated malformations and post operative outcome and 1 year follow up. Ileal loops and ileal loop with meckels being the 2 most common intraoperative finding, timely intervention is effective to prevent long term morbidity [1].
The connecting stalk of the fetus develops blood vessels and fuses with the omphalomesenteric duct to become the umbilical cord approximately 7-8 weeks after conception. By 6 weeks of gestation, two umbilical arteries and two umbilical veins exist. By 8 weeks of gestation, the right umbilical vein regresses, leaving the left umbilical vein as the single vein within the umbilical cord [2].
Hence at birth umbilical cord contains two arteries and one vein, these are covered by Wharton’s Jelly, which is a gelatinous stroma and over all surrounded by single layer of amnion. The left and right umbilical arteries are branches of left and right internal iliac arteries respectively. The arteries carry deoxygenated blood from the fetus to the placenta and the umbilical vein carries oxygenated blood from placenta to the fetus [3].
Umbilical cord may be a location of various congenital anomalies related to morphology, placental insertion, number of vessels, primary tumors etc, single umbilical artery being the commonest finding.
In case of Congenital Umbilical Cord Herniation (CHUC) the umbilical ring does not close and variable portions of the intestines remain in the extracelomic cavity which present at birth as congenital hernia into the umbilical cord. Unlike omphaloceles and gastroschisis, CHUC has an intact abdominal wall, a complete umbilical ring, a sac comprising of outer amnion and inner peritoneal lining and contains contents varying from loops of intestines to any movable intraperitoneal organs [4]. Distinctively a cuff of skin is seen extending from abdominal wall onto the neck of the sac. The abnormality usually takes the form of a globular, asymmetrical swelling situated at the abdominal attachment of the cord and extending into its substance. Sometimes there is a constriction between the swelling and the abdomen. In such a case a serious accident might happen, as in the case described by Victor Bonney et al., where the practitioner removed the hernial sac and its intestinal contents, consisting of small intestine, during the process of ligature and division of the cord at birth. Here we present a study with probably largest sample size on congenital herniation of umbilical cord keeping in view the intraoperative hernia sac contents [5].
Objective
This is an ambispective study, carried out in a tertiary care Govt medical college in Kolkata. The time period was from January 2009 to July 2019. The aim was to evaluate the spectrum of clinical presentation, operative management, associated anomalies, outcome (mortality and morbidity) and short term follow up [6].
Materials and Methods
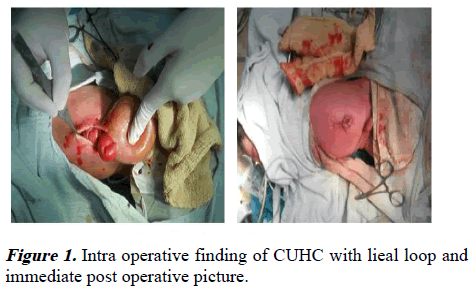
This ambispective study was done on neonates who attended the Out Patient Department (OPD) or emergency department. The babies were evaluated by age, birth weight, gender, any gross clinical malformation. They were also evaluated intraoperatively for any associated anomalies. Post surgery the babies were followed up until 2 years of age in pediatric surgery OPD of the same institute and outcome was recorded (Figure 1) [7].
Results
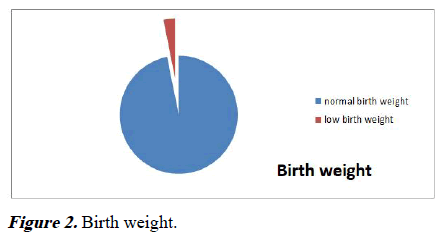
Birth weight
Out of 90 babies, 88 babies (97.77%) had body weight more than 2.5 kg. And rest 2 (2.22%) had bodyweight of 1.5 kg and 1.8 kg (Figure 2).
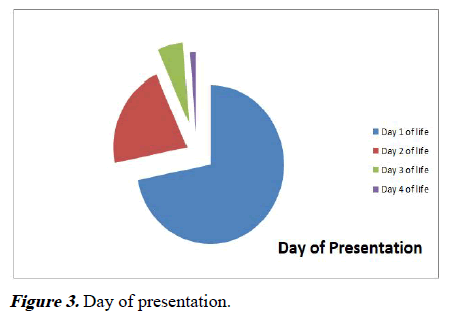
Day of presentation
Among the 90 babies, 64 babies (71.11%) presented on day 1 on life, 19 babies (21.1%) presented on day 2 of life, 5 babies (5.56%) presented on day 3 and 2 babies (2.22%) presented on day 4 of life (Figure 3) [8].
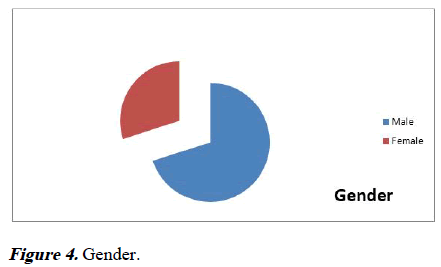
Gender distribution
Out of 90 patients, 63 (70%) patients were male and 27 (30%) patients were female (Figure 4) [9].
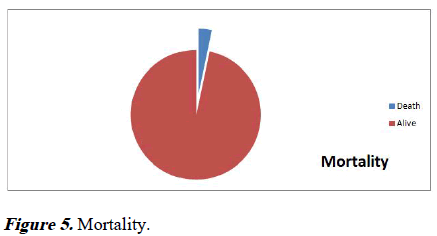
Mortality
3 patients (3.33%) out of these 90 babies expired pre, intra or during post operative follow up (Figure 5).
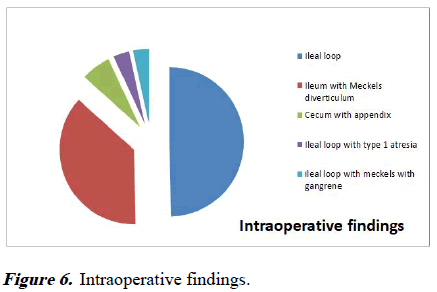
Intraoperative findings
Out of 87 patients (excluding 3 expired babies), who underwent surgery, the following contents of the hernia sac were recorded.
43 patients (49.42%) had ileal loop, 32 patients (36.78%) had ileum with Meckel’s diverticula, 6 patients (6.39%) had cecum with appendix, 3 patients (3.44%) each had ileal loop with type 1 atresia and ileum with Meckels diverticula with gangrene (Figure 6) [10].
Associated findings
Among these 87 patients, there were 2 cases of bilateral undescended testis, 5 babies were diagnosed with Down Syndrome on follow up.
Discussion
CUHC occurs at a specific embryological stage and the cause of failure of return of gut into coelomic cavity is still obscure. Animal experiments and clinical scenerios have clearly described the etiopathogenesis of intestinal atresias. Outcome is variable depending on the co-existing anomalies.
Rahul Gupta et al., reported a case of congenital hernia of umbilical cord associated with type 3 Ileal atresia. We received 3 patients with type 1 ileal atresia, who were operated. Kamalesh Pal reported a case of CUHC with extracelomic colonic atresia with perforation of gut. 3 patients in our study were found to have gangrene of ileal loop. Bilal Mirza et al., published a case series on 3 cases of CUHC, one case was associated with in-utero evisceration of entire small bowel through the presumably ruptured hernia of umbilical cord and other two cases had associated Patent Vitellointestinal Duct (PVID). Most of our cases had ileal loops as content of the hernial sacs. 36.78% cases had meckels diverticulum associated, which is a remnant of Vitellointestinal duct. With prompt identification of the condition and early intervention and adequate post natal care, mortality was reduced to 3.33%. Achiron et al., has showed that CHUC occurs at early embryological stage and this is detectable at early 2nd trimester on antenatal USG, however our study didnot have any of our cases being diagnosed by antenatal USG.
Conclusion
Congenital umbilical cord herniation is a rare but manageable condition when diagnosed early and treated promptly. In our study of 90 cases, we observed a significant reduction in morbidity and mortality through timely surgical intervention and diligent post-operative care. The association with anomalies such as Meckel's diverticulum highlights the complexity of CUHC, underscoring the need for careful intraoperative evaluation. Although antenatal ultrasound can detect CHUC, none of our cases were diagnosed pre-birth, indicating a gap in prenatal screening practices. This study underscores the importance of awareness, early intervention and continued post-surgical follow-up for improving outcomes in neonates with CUHC.
Funding
None.
Conflict of Interest
There is no conflict of interest as stated by authors.
References
- Raju R, Satti M, Lee Q, et al. Congenital hernia of cord: An often misdiagnosed entity. BMJ Case Rep 2015; 2015: bcr2015209642.
[Crossref] [Google Scholar] [PubMed]
- Mirza B, Ali W. Distinct presentations of hernia of umbilical cord. J Neonatal Surg 2016 ;5: 53.
[Crossref] [Google Scholar] [PubMed]
- Sadler TW, Langman J. Langman’s essential medical embryology. 11th edition, Lippincott Williams & Wilkins, 2010, pp. 195-212.
- Predanic M. Sonographic assessment of the umbilical cord. Ultrasound Rev Obstet Gynecol 2005; 5: 105-110.
- Burns CW, Ogryzlo MA. Congenital hernia into the umbilical cord; two cases, one associated with persistent cloaca. Can Med Assoc J 1938; 39: 438.
[Google Scholar] [PubMed]
- Pal K. Congenital hernia of the umbilical cord associated with extracelomic colonic atresia and perforation of gut in a newborn. Afr J Paediatr Surg 2014; 11: 74-76.
[Crossref] [Google Scholar] [PubMed]
- Mirza B, Mirza A, Hashim I, et al. Hernia of umbilical cord: Report of three unusual cases. J Neonatal Surg 2015; 4: 16.
[Google Scholar] [PubMed]
- Achiron R, Soriano D, Lipitz S, et al. Fetal midgut herniation into the umbilical cord: Improved definition of ventral abdominal anomaly with the use of transvaginal sonography. Ultrasound Obstet Gynecol 1995; 6: 256-260.
[Crossref] [Google Scholar] [PubMed]
- Pal K, Ashri H, Al Wabari A. Congenital hernia of the cord. Indian J Pediatr 2009; 76: 319-321.
[Crossref] [Google Scholar] [PubMed]
- Moshiri M, Zaidi SF, Robinson TJ, et al. Comprehensive imaging review of abnormalities of the umbilical cord. Radiographics 2014; 34: 179-196.
[Crossref] [Google Scholar] [PubMed]