Current Pediatric Research
International Journal of Pediatrics
The role of CSF-CRP in diffrentation between bacterial from nonbacterial meningitis.
Qassim Mohammed Hashim, Hidhab Jawad Muhsin, Sahar A Majeed, Jasim Mohammed Hashimand Alaa Maan Johny, Alaa Jumaah Manji Nasrawi*
Department of Pediatrics, Kufa University of Medicine, Najaf, Iraq
- Corresponding Author:
- Alaa Jumaah Manji Nasrawi
Department of Pediatrics
University of Kufa
College of Medicine
Najaf, Iraq
E-mail: alaaj.nasrawi@uokufa.edu.iq
Accepted date: August 21st, 2021
Background: Meningitis is one of dangerous disease in children and the differentiation between acute bacterial and non- bacterial meningitis (particularly viral meningitis) is so important because they differ in their prognosis and treatment. CSF culture and gram stain is ideal for diagnosis but it is coasty and time consuming,so looking for biological markers like CSF-CRP to simplify the accuracy of initial diagnosis of acute meningitis. Objective: To find out the significance of CSF-CRP in patients with bacterial meningitis. Methods: Cross sectional study performed in Babylon teaching hospital on 45 clinically suspected meningitis patients were evaluated for Serum CBC, CRP, Lumbar puncture and CSF examination. Immediately after hospital admission, lumbar puncture and Cerebrospinal Fluid (CSF) examination (bacteriological, cytological and chemical) were done for all patients. Results: CSF-CRP level was remarkably increased in bacterial meningitis (mean 6.59 ± 5.81 mg/l) in comparison with non-bacterial meningitis (mean 1.14 ± 2.36 mg/l), (p<0.001). There are positive relations with WBC and CRP in non-bacterial and bacterial meningitis but this correlation become greatly significant with bacterial meningitis positive groups. Conclusion: This study shows that CSF-CRP can be used for early diagnosis of bacterial meningitis and may be a helpful association in differentiation bacterial and non-bacterial meningitis with CBC and serum CRP.
Keywords
Cerebrospinal fluid, C-reactive protein, Meningitis.
Introduction
Meningitis is one of the serious infections interrelated with remarkable morbidity and mortality (1%-8%) all over the world [1,2]. The definite meningitis incidence in infants and children is not known; anyhow meningitis diagnosis should be express as greatest differential criteria in newborn with change in consciousness level and high fever [3]. Even though viral infection was recorded more than other microbial meningitis bacterial infection is a more serious condition all over the world, especially in developing countries [4-7].
Antimicrobial treatment has large effect on neurologic problems and survival; so early diagnosis of viral from bacterial meningitis or meningoencephalitis is significant for relevant therapy, elimination the resistance to anti-microbial and obtain good results [1,8]. There’re some troubles in viral and bacterial meningitis diagnosis by using usual lab investigations, especially in children like low sensitivity, time taking lab process and change in protein and glucose levels and also cells amount of cerebrospinal fluids due to incorrect and incompetent antibiotic treatment [8,9]. Latex agglutinations are sensitive and fast way for meningitis diagnosis but it’s not routinely used in developing countries [10]. Measuring blood cell count, inflammatory marker, and blood culture were regarded the standard way in diagnosis of bacterial meningitis [11,12]. There’re few biochemical indices in CSF that important in bacterial infection diagnosis like lactate dehydrogenase, lactate, ferritin, c-reactive protein, and cytokines [9,13]. Also lactate of CSF is a possible marker for bacterial meningitis diagnosis but less beneficial if it has low concentration [14].
Broadly speaking we need simple and all inclusive test for the early diagnosis of bacterial meningitis [15]. For ages ago, serum CRP was used to distinguish between viral and bacterial infections in developed countries [16]. Now a days, it has been recommended that measurements of CSF-CRP is dependable, simple and sensitive test for accurate meningitis diagnosis [15,17,18] but it is not a substitute for examination of CSF cytology, biochemistry and culture [15].
In a study by Bansal to approximate CSF-CRP level quantifiably in 121 children with meningitis by immune turbidimetry methods, was achieved that CSF-CRP is a beneficial test to distinguish bacterial meningitis from viral meningitis, tubercular meningoencephalitis and other non-meningitis CNS problems. Also finding of CSFCRP is useful in choosing of correct drugs and the period of therapy [15]. A study by Kalpana, shows that CSF-CRP screening allowed results with a bigger specifically than CRP of blood,so, it can be helpful test used with CSF biochemistry, microbiology and cytology, biochemistry, for diagnoses of meningitis [19].
In study by Bengershom don on children with suspected meningitis, CSF-CRP level close off was obtained as 0.4 mg/L and the specificity and sensitivity and values were 100% and 94%, respectively [20]. Aim of the study was evaluated the diagnostic values of CSF-CRP in patients with bacterial meningitis, and its importance in the differentiation between bacterial and non-bacterial meningitis.
Materials and Methods
Patients
A cross sectional study of patients with age group of (older 1 to 60 months) with suspicion of acute meningitis entered to teaching Hospital in Al-Hilla city in period from September 2019 to January 2020, the demographic and clinical characteristics of patients were recorded on admission. Focused on clinical history and physical examination, those with highly suspicion of acute meningitis were included in the study, those with neurodevelopmental diseases, cerebral palsy, epilepsy, nonspecific febrile illness, malignancy and those with systemic disease rather than CNS were excluded from the study in addition to neonate also excluded. Rapidly after admission, patients were exposed to the followings:
•Full history and clinical examination with large consideration directed to the central nervous system.
•Blood sampling were collected for blood glucose, CBC; was carry out by Sysmex automated hematology analyzer (KX-21N) sysmex corporation KOBE-JAPAN-Serum CRP; which was identified by enzymatic heterogeneous sandwich immunoassay it is a latex agglutination exam for qualitative and semi- quantitative identification of CRP in serum.
•The lumbar puncture was performed by using a sterile lumbar puncture needle and CSF about (1 ml) were examined for WBC counts and differential, proteins and sugar.
Procedure
About 0.5 ml from CSF collected in tube then in deep freezer about (-20°C)to time of evaluation. CSF sampling was evaluated for CRP by simple Ag-Ab precipitation tests, latex slide agglutination way with the help of financially obtainable kit produced by Salucea, Span diagnostics. The qualitative and semi quantitative test was performed on the collected sampling by blending CSF drop with drop of latex reagent on a slide and both were blended softly. The deposition of clear agglutination within 2 minutes indicate positive test and CSF-CRP concentration more than 6 mg\l, then CSF diluted (1:2 ect, 1:4 ect, 1:8 ect) in 0.9g\L saline fluid and add one drop of positive control.
The CSF-CRP titer can considered as the biggest dilutions showing a positive result. The estimated CRP level(mg\l) found in the sample can be calculated by the equation:
CRP titer=Highest dilution with positive reaction × Reagent sensitivity (6 mg\l)
No agglutination considered negative test in values less than 6 mg\l. Depending on leukocyte count in CSF analysis, the patients were divided into two groups: Group I (29 patients) have more leukocytes count in CSF (100-1000\mm3) especially PMN of higher than 50%, level of CSF glucose lower than 2/3 blood glucose and level of CSF protein of 100-500 mg\dl, suggested bacterial meningitis and Group II (16 patients) with CSF pleocytosis of lower than 100/mm3 with lymphocytes predominant, level of protein 50-200 mg/dl and normal glucose suggested non-bacterial meningitis.
Statistical analysis
Data were entered, checked and analyzed using version 20.0 SPSS (Statistical Package for the Social Sciences, Chicago, IL), data were expressed as percentage and number for qualitative variables and mean ± standard deviation for quantitative ones. P~0.05 was considered significant.
Results
The clinical and demographic features of the studied patients were re summarized in Table1 and shows that, total number of included patients was 45 cases, 26 were males and 19 were females their age was ranging from 1momth to 60 months mean of age was 18.78. Clinical presentation of patients at time of admission, most included patients had fever (95.5%), convulsions (73.3) and vomiting (93.3%) as shown in Table 1.
| Age | Mean | 18.78 |
| Range | 59 | |
| Standard deviation | 18.63 | |
| Sex | Male | 26 |
| Female | 19 | |
| Male: Female ratio | 1.368:1 | |
| C/F | Fever | 43 (95.5%) |
| Vomiting | 42 (93.3%) | |
| Convulsion | 33 (73.3%) | |
| Irritability | 23 (51.1%) | |
| Lethargy | 16 (35.5%) | |
| Bulging fontanel | 16 (35.5%) | |
| Neck stiffness | 12 (26.6%) | |
| Headache | 12 (26.6%) | |
| Dis. LOC | 8 (17.7%) | |
| Photophobia | 4 (8.8%) | |
| Skin rash | 8 (17.7%) | |
| Kerning | 2 (4.4%) |
Table 1. Characteristics and clinical pictures of included patients.
The mean CSF neutrophil count in all study groups was (35.38 ± 79.62) and means CSF lymphocytes count (14.28 ± 23.92) as shown in Table 2 which represents all CSF and CBC measurement.
| Parameter | Mean | St. deviation |
|---|---|---|
| Neutrophils in CSF | 35.38 | 79.62 |
| Lymphocytes in CSF | 14.28 | 23.92 |
| Proteins in CSF | 441.69 | 429.35 |
| Sugar in CSF | 52.9 | 19.57 |
| Total WBC in blood | 14.23 | 7.2 |
| Neutrophils% | 58.16 | 16.46 |
| Lymphocytes% | 31.39 | 15.83 |
| HB% | 11.81 | 1.41 |
| HTC% | 36.25 | 5.74 |
Table 2. CSF and blood finding of all included patients.
According CSF cytological and biological, the included patients were categorized into two groups as shown in Table 3: Group 1 (29 Patients with bacterial meningitis, 17 were males and 12 were female, age ranging from 1-60 months, mean of age was 20.84) and Group 2 (16 patients with non-bacterial meningitis, 9 were males and 7 were female, age ranging from 1-36 months, mean of age was 14.65).
Distribution of clinical features, age and gender of both bacterial and non-bacterial meningitis also show in Table 3.
| Variables | Patients with bacterial meningitis (N=29) | Patients with non-bacterial meningitis (N=16) | P-value |
|---|---|---|---|
| Age in months | |||
| Mean | 20.84 | 14.65 | |
| Range | 59 | 35 | 0.4 |
| Standard | 21.14 | 11.56 | |
| Sex | |||
| Male number | 17 | 9 | |
| Female number | 12 | 7 | 0.87 |
| Male: Female ratio | 1.41 | 1.28 | |
| Fever | 28 (96%) | 15 (93.7%) | 0.45 |
| Vomiting | 27 (93%) | 15 (93%) | 0.91 |
| Convulsion | 23 (79%) | 10 (62%) | * 0.04 |
| Irritability | 13 (44%) | 10 (62%) | 0.25 |
| Lethargy | 12 (41%) | 4 (13%) | 0.27 |
| Bulging fontanel | 11 (37%) | 5 (31%) | 0.65 |
| Headache | 7 (24%) | 5 (31%) | 0.08 |
| Neck stiffness | 8 (27%) | 4 (13%) | 0.06 |
| Photophobia | 4 (13%) | 0 (0%) | 0.12 |
| Dis. LOC | 3 (10%) | 5 (31%) | 0.07 |
| Skin rash | 3 (10%) | 5 (31%) | 0.07 |
| Kerning sign | 2 (6%) | 0 (0%) | 0.22 |
Table 3. Characteristics and clinical features of bacterial and non-bacterial patients.
Convulsion was seriously higher in bacterial groups than those of non- bacterial groups as shown in Table 3.
Regarding CSF parameters: mean of neutrophils in CSF of patients with bacterial meningitis was 55.11 against 0.67 in non-bacterial meningitis p~0.05, lymphocytes mean was 15 in bacterial meningitis and 12.94 in non-bacterial meningitis, proteins level mean was higher in bacterial than in non- bacterial meningitis (571.16, 204.89 respectively) p~0.05. Sugar level in CSF of patients with non- bacterial meningitis was higher than those of bacterial meningitis with mean of 44 for bacterial and 71.52 for non-bacterial meningitis as show in Table 4.
| Parameter | Bacterial meningitis (N=29) mean ± SD | Non-bacterial meningitis (N=16) mean ± SD | P-value |
|---|---|---|---|
| Neutrophils lumm | 55.11 ± 95 | 0.67 ± 0.853 | 0.003 |
| Lymphocytes lumm | 15 ± 31.65 | 12.94 ± 4.59 | *0.01 |
| Proteins mg/dl | 571.16 ± 486.13 | 204.89 ± 102.132 | *0.04 |
| Sugar mg/dl | 44 ± 15.5 | 71.52 ± 16.61 | *0.05 |
Table 4. Categorization of the studied patients to bacterial and non- bacterial meningitis according to CSF parameters.
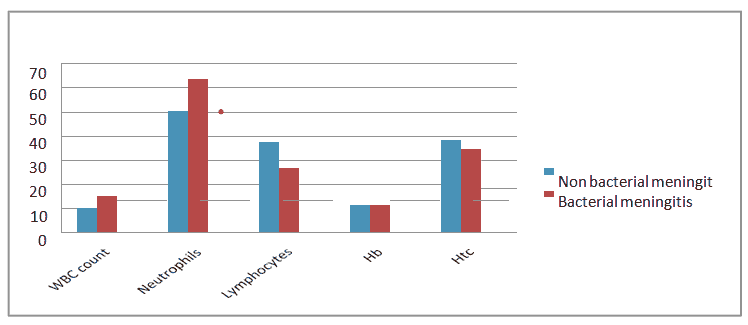
Regarding blood lab findings, the results show statistically significant difference in leukocyte count in bacterial meningitis in contrast with those of non-bacterial meningitis (P-value~0.009). The same result for neutrophils (P-value~0.05) but was not significant for lymphocytes. As shown in Figure 1 and Table 5.
| Parameters | Bacterial Meningitis (N=29) Mean ± SD | Non- bacterial meningitis (N=16) Mean ± SD | P-value |
|---|---|---|---|
| WBC count | 15.08 ± 6.97 | 10.29 ± 3.51 | 0.009 |
| Neutrophils% | 63.89 ± 14.59 | 50.29 ± 19.93 | *0.01 |
| Lymphocytes% | 26.88 ± 12.65 | 37.6 ± 18.17 | 0.51 |
| HB% | 11.58 ± 1.527 | 11.64 ± 0.95 | 0.81 |
| HTC% | 34.84 ± 5.52 | 38.25 ± 5.42 | 0.44 |
Table 5. Categorization of patients according to blood parameters.
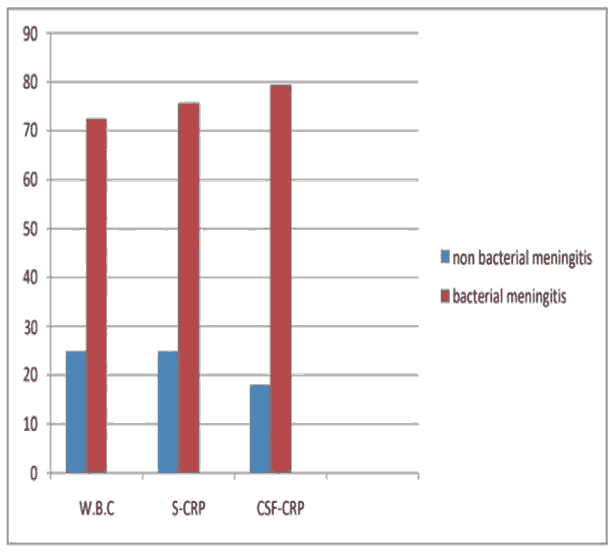
CRP level had significant difference between patient with bacterial meningitis,(mean 6.59 ± 5.81 mg/l) and in patients with non-bacterial meningitis (mean 1.14 ± 2.36 mg/l) (P=0.03) as show in Table 6 and Figure 2.
| CSF-CRP mg/l | Total patients (n=45 y) | Bacterial meningitis (N=29) | Non bacterial meningitis (N=16) |
|---|---|---|---|
| Mean | 4.58 | 6.59 | 1.14 |
| St. Deviation | 5.72 | 5.81 | 2.36 |
Table 6. CSF-CRP level among the studied patients.
There are positive relationships between CSF-CRP, TLC and serum CRP especially in suspected bacterial meningitis group as show by Table 7.
| Parameter | Bacterial meningitis (N=29) | Non- bacterial meningitis (N=16) | P-value |
|---|---|---|---|
| WBC | |||
| Leukocytosis (%) | 21(72.4%) | 4(25%) | *0.02 |
| Non-leukocytosis (%) | 8(27.5%) | 12(75%) | |
| CRP: Serum | |||
| Positive (%) | 22(75.8%) | 4(25%) | *0.0 01 |
| Negative (%) | 7(24.1%) | 12(75%) | |
| CSF-CRP | |||
| Positive | 23(79.3%) | 3(18%) | *~0. 001 |
| Negative | 6(20.6%) | 13(81.2%) | |
Table 7. Distribution of CSF and blood parameter in patients with bacterial and non-bacterial meningitis.
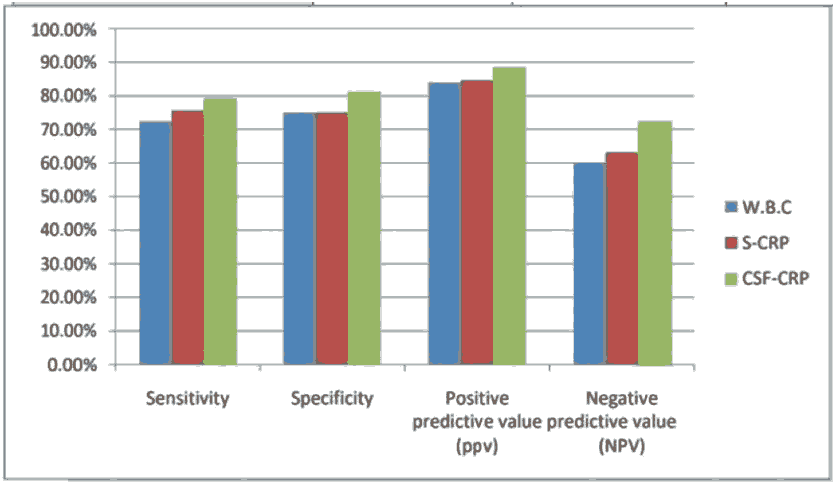
Our comparison between serum CRP, WBC count and CSF-CRP in the studied patients revealed that CSF-CRP had higher sensitivity, specificity, negative and positive predictive value than serum CRP and WBC count for bacterial meningitis diagnosis as show in Table 8 and Figure 3.
| Validity test | WBC count | S-CRP | CSF-CRP |
|---|---|---|---|
| Sensitivity | 72.40% | 75.80% | 79.30% |
| Specificity | 75% | 75% | 81.40% |
| Positive predictive value | 84% | 84.60% | 88.40% |
| Negative Predictive Value (NPV) | 60% | 63.10% | 72.20% |
Table 8. Validity tests of WBC, serum CRP and CSF-CRP for diagnosis of meningitis.
Discussion
Meningitis cause is still a problem as the biochemical and clinical features is usually beclouded due to prior antibiotic abuse. It became difficult to separate the organism from CSF or blood. However, culture of CSF is positive in 30%–60% of cases only, according to many studies. In many areas, facilities to isolate CSF or blood organisms is deficient and, if it is founds, it takes long time for culture results [9].
There is no rapid and precise test to diagnose the Cause of meningitis.No definite interpretation of CRP emigration to CSF was accessible in the literatures. CSF-CRP absorption was lesser than that of serum in several folds. This difference was interpreted by direct CRP liver excretions into serum which then go through ultra-filtration to form CSF concentrate. Circulating of serum globulin and albumin through affected meninges was explained and it shows possible that CRP may pass from plasma to CSF in a same way. In bacterial meningitis the major cell were polymorph missing the site of attachment of CRP molecule in the affected tissue privilege more CRP to-gathered in the CSF which identified by CRP test [21]. The reality was noticed in our study in suspicion of meningitis who consequently shows noticeable CSF-CRP should be announced as bacterial meningitis.
In relation to other widely used test, CRP appears to be a more specified and précised marker in various infections such as meningitis. In this study we found that, according to epidemiological factors bacterial meningitis had male predominance as in Sharad et al. study [22,23]. And according to clinical pictures we found that the most common symptoms in bacterial meningitis are fever 96%, vomiting 93%, convulsion 79%, while in Piyush et al. study fever was 83%, vomiting 33% and convulsion 83% [24]. In late study, relative neck rigidity was more in bacterial meningitis and disturbed consciousness more in non-bacterial meningitis, as our study.
Also we found that there was very discrete union of bacterial meningitis with leukocytosis and PMN predominance72% this result was agree with Piyush et al. study was 83% and 85% respectively [24,25]. Increased protein and decreased sugar concentration were prominent in bacterial meningitis same result in Piyush et al. studies [24,26]. One of the important results of the present study was the remarkable increased of S- CRP levels in patients have bacterial meningitis than in those with non-bacterial meningitis 75% and 25%, like that serum CRP levels 82% and 30% respectively in Russul study [27].
Conclusion
In a final we found that CSF-CRP level was increased in group of patients with bacterial meningitis 79% while in those with non-bacterial meningitis patients 18%, in Hiader study CRP in CSF was positive in 77% in bacterial and 6% in non-bacterial meningitis. In our study, the sensitivity and specificity of CSF-CRP in the diagnosis of bacterial meningitis was found 79% and 81%, lower than other studies where (sensitivity 77%-specificity 93%) in Hiader study, (sensitivity 96%-specificity 100%) in Russul study.
Recommendation
It was recommended that CSF-CRP need to be available in the emergency lab to be used in early differentiation between bacterial and non-bacterial meningitis.
Limitation
CSF-CRP was estimated by semi quantitative methods. Therefore, the exact values of CRP could not be detected. With good laboratory facilities detection of the precise CRP level could decline our study limitation.
References
- Corrall CJ, Pepple JM, Moxon ER, et al. C-reactive protein in spinal fluid of children with meningitis. J Pediatr 1981; 99(3): 365-9.
- Swartz M. Acute bacterial meningitis. Infectious diseases 1998; 1: 1160.
- Krogstad P, Feigin RD, Cherry JD, et al. Textbook of pediatric infectious diseases. Osteomyelitis and septic arthritis. Saunders 2004.
- Attia J, Hatala R, Cook DJ, et al. The rational clinical examination. Does this adult patient have acute meningitis? JAMA 1999; 282(2): 175-81.
- Logan SA, MacMahon E. Viral meningitis. BMJ 2008; 336(7634): 36-40.
- Carbonnelle E. Laboratory diagnosis of bacterial meningitis: Usefulness of various tests for the determination of the etiological agent. Med Mal Infect 2009; 39(7-8): 581-605.
- Brouwer MC, Tunkel AR, van de Beek D. Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis. Clin Microbiol Rev 2010; 23(3): 467-92.
- Cho SH, Lee HB, Lee KS. Clinical study of cerebrospinal fluid lactate levels in children with menigitis. J Korean Pediatr Soc 1984; 27(5): 475-82.
- Straus SE, Thorpe KE, Holroyd-Leduc J. How do I perform a lumbar puncture and analyze the results to diagnose bacterial meningitis?. JAMA 2006; 296(16): 2012-22.
- Sanya E, Taiwo S, Azeez O, et al. Bacterial meningitis: Problems of empirical treatment in a teaching hospital in the tropics. Internet J Infect Dis 2006; 6(1): 1-8.
- Tunkel AR, Hartman BJ, Kaplan SL, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis 2004; 39(9): 1267-84.
- Chaudhuri A, Martin PM, Kennedy PGE, et al. EFNS guideline on the management of community-acquired bacterial meningitis: report of an EFNS Task Force on acute bacterial meningitis in older children and adults. Eur J Neurol 2008; 15(7): 649-59.
- Bullen JJ, Rogers HJ, Griffiths E. Role of iron in bacterial infection. Curr Top Microbiol Immunol 1978; 80: 1-35.
- Lindquist L,Linne T, Hansson LO, et al. Value of cerebrospinal fluid analysis in the differential diagnosis of meningitis: a study in 710 patients with suspected central nervous system infection. Eur J Clin Microbiol Infect Dis 1988; 7(3): 374-80.
- Bansal S, Gupta R, Gupta PP, et al. Quantitative levels of C-reactive protein in cerebrospinal fluid in children with bacterial and other meningitis. J Evol Med Dent Sci 2013; 2(25): 4594-8.
- Peltola H. C-reactive protein for rapid monitoring of infections of the central nervous system. Lancet 1982; 319(8279): 980-3.
- Nagarathna S, Veenakumari HB, Chandramuki A. Laboratory diagnosis of meningitis. Meningitis. In Tech 2012.
- Kawamura M, Nishida H. The usefulness of serial C-reactive protein measurement in managing neonatal infection. Acta Paediatr 1995; 84(1): 10-3.
- Malla KK, Malla T, Rao KS, et al. Is cerebrospinal fluid C-reactive protein a better tool than blood C-reactive protein in laboratory diagnosis of meningitis in children?. Sultan Qaboos Univ Med J 2013; 13(1): 93-9.
- Gershom EB, Briggeman-Mol GJ, de Zegher F. Cerebrospinal fluid C-reactive protein in meningitis: Diagnostic value and pathophysiology. Eur J Pediatr 1986; 145(4): 246-9.
- Konstantinidis T, Cassimos D, Gioka T, et al. Can procalcitonin in cerebrospinal fluid be a diagnostic tool for meningitis?. J Clin Lab Anal 2015; 29(3): 169-74.
- Banasal S, Gupta R, Gupta PP, et al. Quantitative levels of CRP in CSF in children with bacterial and other meningitis. J Evol Med Dent Sci 2013; 2: 4594-8.
- Uddinl MB, Rahman M, Siddique AB. Usefulness of CRP in differentiating pyogenic and aseptic meningitis. TAJ 2009; 22: 78-81.
- Sadat P, Patel SV, Krutishsh. Role of CSF-CRP as a bedside diagnostic test in children with meningitis: NHL. J Med Sci 2013; 2: 54-6.
- Khanam R, Hanif M, Hoque MDM, et al. Role of CSF-CRP for the differentiation of bacterial from aseptic meningitis in children. Bangladesh Child Health 2012; 36: 126-32.
- Hiader N. Acute Meningitis in children. Clincal and Laboratory Profiles. QMG 2013; 9: 119
- Russul FM. The significance of C-reactive protein in childhood acute meningitis. J Babylon 2015; 12: 730-8.