Current Pediatric Research
International Journal of Pediatrics
Severe juvenile dermatomyositis with specific liver involvement onset concomitant with COVID-19 infection: A case report.
Nesrine Jammeli1*, Nouha Ben Abedeljelil2, Bahri Mahjoub1
1Department of Pediatrics, Taher Sfar Hospital, Mahdia, Tunisia
2Department of Histopathology, Fattouma Bourguiba Hospital, Monastir, Tunisia
- Corresponding Author:
- Nesrine Jammeli
Department of Pediatrics,
Taher Sfar Hospital,
Mahdia, Tunisia
E-mail: nesrine.jammeli@gmail.com
Received: 27 March, 2023, Manuscript No. AAJCP-23-92479; Editor assigned: 29 March, 2023, Pre QC No. AAJCP-23-92479(PQ); Reviewed: 07 April, 2023, QC No. AAJCP-23-92479; Revised: 17 April, 2023, Manuscript No. AAJCP-23-92479(R); Published: 27 April, 2023, DOI:10.35841/0971-9032.27.04.1185-1189
Juvenile Dermatomyositis (JDM) is an autoimmune disease that involves skin, muscle and internal organ disorders. Its mechanisms still not well established, but the triggering role of viral infections has been described. In this context, the effect of the COVID-19 on the onset of autoimmune disorders such as JDM remains a matter of study and research. We report a severe JDM, following a confirmed COVID-19 infection in a previously healthy 8 year-old boy who presented with various skin lesions and a cholestatic liver involvement. Laboratory findings were consistent with an inflammatory myositis and an autoimmune liver disease. Skin and muscle biopsies confirmed the diagnosis of JDM. The therapy choice was difficult. Finally, he received a second line therapy of the JDM with a favorable outcome. The liver fragment analysis showed a steatosis. This case supports the hypothesis of COVID-19 triggering role in the genesis of JDM and autoimmune diseases.
Keywords
Juvenile dermatomyositis, Myositis, Autoimmune, Liver
Introduction
Few recent publications suggested COVID-19 as a possible trigger of autoimmune diseases, namely; Juvenile Dermatomyositis (JDM) [1,2]. In this pathology, internal organ involvement is common. Associated with COVID-19, several reported cases presented with severe organ lesions such as neuromyositis and fatal interstitial lung disease [1,3]. In this manuscript, we report a case of COVID-19 induced JDM associated with a liver damage that was challenging to differentiate from a liver autoimmune disease.
Case Presentation
An 8 year-old boy was admitted to investigate a one-month history of poor general state, weight loss, fatigue, skin lesions and liver cytolysis discovered on his laboratory findings. His medical history was uneventful except for a COVID-19 infection documented with the symptoms onset. Physical examination showed a low grade fever of 38.3°C and a eutrophic child. He had hepatomegaly without associated jaundice or splenomegaly.
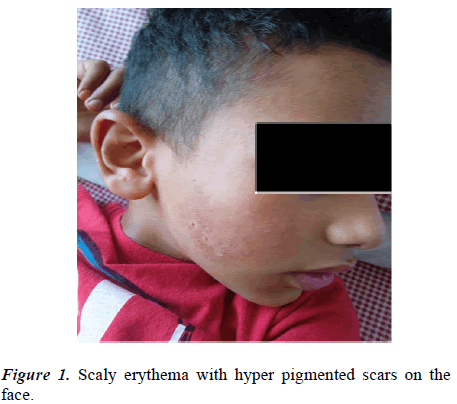
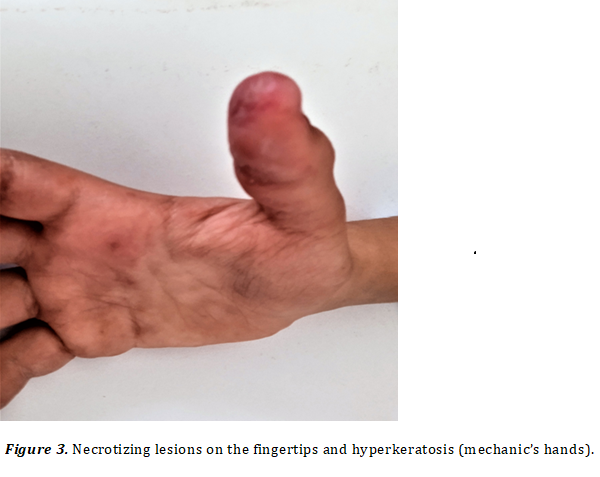
A skin examination objectified scaly heliotrope eyelids and cheeks leaving hyper pigmented scars (Figure 1). We also noted desquamative firm lesions of few millimeters at the joint extensors suggesting Gottron papules (Figure 2A and 2B). A musculoskeletal examination revealed a positive Gower sign manifested by weakness of proximal muscles of both upper and lower limbs. Muscle power in these areas was 3/5. These signs were rapidly followed by a difficulty to walk, arthritis and calcinosis on the knees and the elbows. Moreover, he developed a solid dysphagia, occipital alopecia and necrotizing lesions on the fingertips and palmar hyper keratosis suggestive of ‘mechanic’s hands’ (Figure 3).
On the biological assessment, the cell blood count showed a hypochromic and microcytic anemia of 10.6 g/dl, a hyper ferritinemia of 375 ng/ml (N:11-25 ng/ml). The liver biological findings revealed a cytolysis with alanine and aspartate transferase at 573 and 325 UI/l respectively. Furthermore, the gamma-glutamyl transferase was elevated up to 118 UI/l (N: 25-50 UI/l). Kidney function and serology of hepatitis were within normal limits. Despite normal muscular biological tests, muscular involvement was documented by electromyography showing myopathic pattern and suggesting inflammatory myositis.
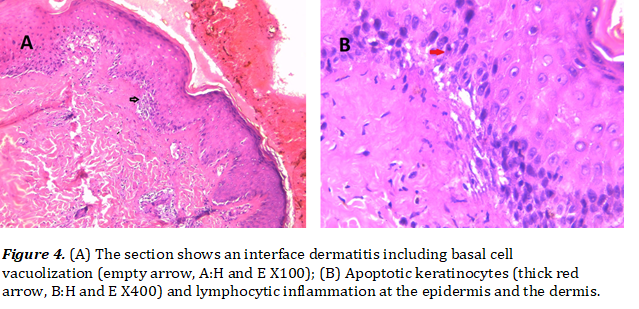
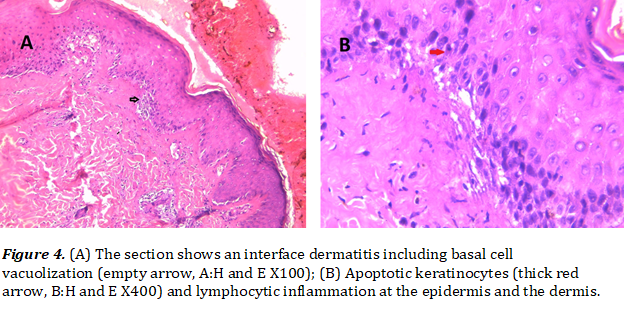
An autoimmune assessment revealed positive, antinuclear antibodies at a level of 1/180 consisting of anti DNA, anti ENA, anti SSA and the patient was positive for anti Ro-52 and smooth muscle antibodies (1/50). Therefore, a liver biopsy was scheduled and an overlap syndrome was evoked. However, lupus anticoagulant and rheumatoid factors were negative and labial gland biopsy was also normal. However, damaged skin biopsy was suggestive of JDM, showing a basal skin focally vacuolated with apoptotic keratinocytes and dermal perivascular lymphocytic infiltration (Figures 4A and 4B).
The muscular biopsy objectified atrophic and degenerating muscle bundles infiltrated by lymphocytes and rare neutrophils consistent with the diagnosis of a JDM. In this context, complementary assessment including ophthalmic examination, urine strip test, chest radiography and echocardiogram was normal. A chest computed tomography showed 2% ground glass opacities related to COVID-19.
On the basis of the EULAR/ACR criteria for adult and juvenile idiopathic inflammatory myopathies, it was a definite case of JDM (score=12). Before any medication was administered, a liver biopsy was performed and the patient was, then, treated with five pulses of methyl prednisolone relayed by oral corticotherapy, hydroxychloroquine and azathioprine. Later, the liver histopathological section revealed a steatosis affecting about 5% of the organ. After 6 months of treatment and physiotherapy courses, the outcome was good. The patient could walk normally and climb stairs. His skin lesions healed and he had normalized liver biology.
Results and Discussion
The current case report a JDM appeared concomitantly with a COVID-19 infection. The repercussion on the general state was significant and except for the mechanic’s hands, the skin involvement was classic. This sign is widely described in adults in association with severe interstitial lung disease and few pediatric cases were published [4,5]. Moreover, this finding is in accordance with several authors such as Rodero, et al. who had reported two cases of JDM onset and relapse due to SARS-COV-2 infection [2].
According to the literature, cytolysis is the most common liver disease in JDM [6]. To our knowledge, hepatic steatosis, as a complication of JDM, is rare in children. Russo, et al. reported the first 3 cases of cholestatsis in JDM; a mild fatty degeneration was present in all the patients [7]. Moreover, extensive liver fatty degeneration with JDM was fatal in few previously described cases [5,8]. In the present case report, we described a mild form of liver cholestatic involvement in JDM that was associated with autoimmunity. In this context, the main mechanism behind is a treatment-induced liver toxicity or an inflammatory systemic involvement [9,10].
We found only one 3-year old pediatric case had been reported with an effective type 2 autoimmune hepatitis followingCOVID-19 infection [10]. In fact, the positivity of anti-smooth muscle antibodies without histopathological liver autoimmune lesions in our patient was consistent with the hypothesis of COVID-19 triggering role of autoimmunity. The authors concluded a double mechanism; a systemic autoimmune hyper stimulation involving inflammatory cytokines, namely, Tumor Necrosis Factor (TNFα), Inter Leucine (IL)-1 and IL-6. The second mechanism is a molecular resemblance between the virus and liver antigens [11,12].
Conclusion
Finally, our case provides supplementary evidence that COVID-19 infection could trigger autoimmune diseases as JDM and autoimmune responses. Diversity of the proposed mechanism for COVID-19 induced internal organs could make the patient undergo an invasive exploration such as liver biopsy. In our case, liver damage was uncommon and decisive in the choice of treatment. In fact, the first line treatment recommended for JDM is based on corticosteroids associated with methotrexate. This last molecule represents the second line therapy in autoimmune hepatitis. Therefore, we opted for treating our patient with corticosteroids and azathioprine and the outcome was favorable.
Funding
No funding was provided for this study.
Conflict of Interest
The authors have no conflicts of interest to declare.
Ethical Statement
Written informed consent was obtained from the legal guardian for the anonymized case details and accompanying images to be published. A copy of the written consent is available for review by the editorial office of this journal.