Current Pediatric Research
International Journal of Pediatrics
Searching the CMV infection (CMV Ag65 in blood; and CMV-DNA (PCR in perilymphatic fluid) in children with cochlear implant surgery: A cross sectional study in Tehran, Iran.
Samileh Noorbakhsh1, Mohammad Farhadi2, Moteza Haghighi3, Zahra Movahedi4, Hesamodin Emam Jomeh2 and Sarvenaz Ashouri2
1Pediatric Infectious Diseases Department, Iran University of Medical Sciences, Tehran, Iran.
2ENT – Head and Neck Research Center, Iran University of Medical Sciences, Tehran, Iran.
3Research Center of Pediatric Infectious Diseases, Iran University of Medical Sciences, Tehran, Iran.
4Pediatric Infectious Diseases Department, Qom University of Medical Sciences and Health Services, Qom, Iran.
- *Corresponding Author:
- Samileh Noorbakhsh
Pediatric Infectious Diseases Ward
4th floor Hazrat Rasul Hospital, Niayesh Street
Satarkhan Avenue, Tehran, 14455
Islamic Republic of Iran.
Tel: 098-21-66525328
Fax: 098-21-66525328
E-mail: Samileh_noorbakhsh@yahoo.com
Accepted date: May 18, 2017
Background: Prevention and early treatment of congenital CMV infection have a high priority in our country. The main goal of this study was to search the CMV Ag65 in blood and CMVDNA (PCR) in perilymphatic fluid of children undergone to cochlear implant surgery. Methods and materials: A cross sectional study (2012-2014) designed in Rasoul Akram hospital referral centre in Tehran, Iran. Thirty nine cases with cochlear implant surgery (mean age=2.37+2.16 years) evaluated for CMV infection. One ml of the whole blood were obtained from cases before surgery and searched for CMV antigen p65. Also perilymphatic fluid were taken during surgery and searched for CMV-DNA by PCR method. The results compared. Chisquare values (CI: 95%; P<0.05) were calculated. P value<0.05 was considered significant. Results: Positive CMV-Ag 65 detected in 43% (18/39), positive CMV-PCR were found in 26.7% (10/39) of cases. A poor agreement was found between 2 methods for CMV infection in cases. Sensitivity and Specificity, PPV and NPV for CMV antigenemia (p65) in compare with positive CMV DNA (PCR) in perilymphatic fluid were 43%, 54%, 77% and 65%, respectively. The mean age of cases with positive and negative CMV PCR was meaningful (p?0.001) but not for CMVantigen p 65 (p=0.3). No correlation between positive CMV results (both methods) and positive clinical signs for CMV infection (except SNHL) were observed (p=0.4, 1). Conclusion: Universal screening of newborns for congenital CMV and longitudinal audiometric follow-up are needed for all confirmed CMV infected cases. We prefer to consider CMV seropositive SNHL children (<1 year old) as congenital form. We recommend a complete DNA assay in blood for CMV infection to differentiate the congenital from the acquired infection in seropositive (CMV-IgM) cases after first birth day. Treatment of CMV infection can diminish occurrence of SNHL.
Keywords
Sensory neural hearing loss (SNHL), Cochlear implant, CMV antigen, P65.
Introduction
Sensory Neural Hearing Loss (SNHL) may develop at birth (congenital) or later in life (acquired). Congenital SNHL is most often due to genetic or infection passes from mother to her baby [1-3]. Congenital CMV is the most common cause of nonhereditary SNHL in children [2]. Up to 50% of maternal CMV infections have nonspecific clinical manifestations and most remain undetected unless specific serological testing is undertaken [1,2]. Approximately 11% of infants born with congenital CMV infection are symptomatic (jaundice, splenomegaly, petechiae, microcephaly, intrauterine growth restriction and death). Congenital CMV infection may cause severe long-term sequelae, including progressive SNHL and developmental delay in 40-58% of symptomatic neonates and ~14% of initially asymptomatic infected neonates [2-4].
Usually, despite of being the leading infectious cause of congenital malformation, congenital CMV is unrecognized [3]. Universal screening of newborns for congenital CMV infection should be initiated and combined with longitudinal audiometric follow-up [4-6]. Reliable estimates of the long-term outcome of congenital CMV infection are mandatory to increase vigilance, especially among pregnant women and to draw attention to preventive measures, vaccine development and prenatal and postnatal therapy [5,6]. Ogawa et al. [4] described that not all patients diagnosed with congenital infection using umbilical cord assay were found to be positive for CMV-DNA by perilymphatic fluid assay. In addition, a CMV-DNA-positive result was observed in one patient who had not been diagnosed with congenital infection [3]. Recently, Goderis et al. [5] longitudinally reported that SNHL happened in 63% of symptomatic congenital CMV and 8% of asymptomatic ones. Delayed-onset SNHL occurred in 10.6% of symptomatic and 7.8% of asymptomatic congenital CMV, 29.3% of symptomatic group and 1.6% of asymptomatic children used some kind of hearing amplification [5]. Yamamoto et al. [6] reported 1% of newborns were infected with CMV by PCR and10% had symptomatic infection at birth. SNHL was observed in 9.8% in 12 months age [6]. Profound loss (>90 db) reported in 4/5 children with bilateral SNHL while 5 children with unilateral loss had moderate to severe deficit. The presence of symptomatic infection was independently associated with SNHL after adjusting for intrauterine growth restriction, gestational age, gravidity and maternal age [6].
Diagnosis of congenital CMV infection at birth or in the first 3 weeks of an infant's life is crucial, as this should prompt interventions for prevention of delayed-onset hearing loss and neurodevelopmental delay in affected infants [7-10]. The application of a noninvasive serological assay to detect CMV infection would be advantageous for asymptomatic newborns, though it could not change the outcomes of pregnancy [11,12]. Prevention strategies should also target mothers because increased awareness and hygiene measures may reduce maternal infection. Recognition of the importance of CMV in pregnancy and in neonates is increasingly needed, particularly as therapeutic and preventive interventions expand for this serious problem [12-14]. Naing et al. [15] reviewed the prevalence, clinical features, diagnosis and prevention the congenital CMV in pregnancy. Symptomatic infants are at increased risk of developing permanent sequelae, including neurodevelopmental delay and SNHL [11,12].
Scott et al. [14] determined that until yet strategies to prevent congenital or maternal CMV infections failed to yield positive results. Use of CMV hyper immune globulin and development of a maternal vaccine, treatment with Gancyclovir when CMV infection is diagnosed in the early life is recommended and is associated with diminished occurrence of SNHL. Probably, antiviral therapy with intravenous Gancyclovir in neonates or 6 months of oral valganciclovir improves hearing and neurodevelopmental outcomes at least in symptomatic infants [11-14].
Some Iranian authors reported the seroprevalence of CMV infection in Iranian pregnant women [7-9]. Like as other parts of world, CMV is the most common cause of intra uterine infection in Iran. Also, CMV was the most common infectious agents in SNHL children compared to the healthy children. Probably both congenital and acquired CMV can induce progressive hearing loss in our cases [10-13].
In our country, cochlear implant surgery is needed for some SNHL cases with various etiologies. Idiopathic SNHL and its prognostic factors have also been discussed in many references [10-13].
Prevention and early treatment of congenital CMV infection have a high priority in our country.The main goal of this study is searching the CMV Ag65 in blood and also CMV-DNA (PCR) in perilymphatic fluid in children with cochlear implant surgery for determining the role of CMV infection to developing the SNHL.
Methods and Materials
In this cross sectional study, we studied 39 children were candidate for cochlear implant surgery in Rasoul Akram Hospital affiliated by IUMS in Tehran (2010-2014) who were between 6 months-14 years; mean age=2.37+2.16 years; 52.6% (n=20) of patients were male and 44.7% (n=17) were female. This cross-sectional study was approved by the Ethical Committee in Research Center of Pediatric Infectious Diseases affiliated by Iran University of Medical Sciences. Consent letter obtained from all cases. An authorized physician completed the questionnaire for each case.
Blood samples (2 ml) were obtained on the day before surgery for searching the CMV antigen p65.The blood samples (1 ml) were centrifuged and sera transferred to our research laboratory, were kept frozen at -20°C until usage. 1 ml of blood searched for CMV p65 antigen. Perilymphatic fluid during surgery were obtained by surgeon and collected into sterile microtubes, then and kept in freezer for checking CMV PCR.
Lab Test
Serological tests: Specific antibodies (IgM and IgG) against CMV were determined in the serum by commercial kits (BiochemImmunosystems, Bologna, Italy). The results were calculated qualitatively and interpreted by cut-off controls according to the manufacturer’s instructions.
PCR: On Perilymphatic samples, DNA extraction was done using a PCR template purification kit (NucleoSorb, Quiagen). The quantification kit for detection of the CMV genomes (PrimerDesign™ using the TaqMan® principle) was done.
Statistical Analysis
The Student t-test was used to determine significant differences in means for all continuous variables. Chisquare values (CI: 95%; P<0.05) were calculated for all categorical variables. P value less than 0.05 was considered significant. All analyses were conducted using SPSS version 13.
Results
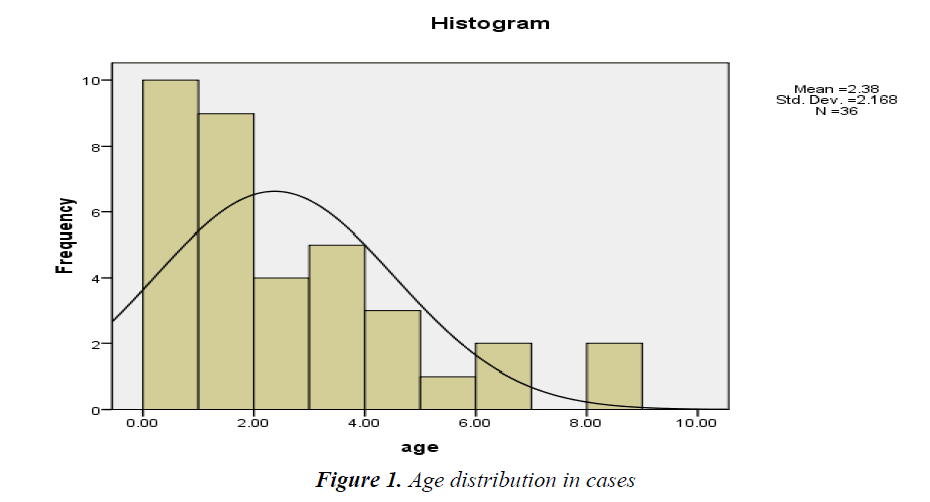
Age distribution of cases showed in Figure 1.
Positive CMV-Ag 65 detected in 43% (18/39), positive CMV-PCR were found in 26.7% (10/39) of cases.
Comparison the age and clinical signs between 2 methods showed in Tables 1 and 2.
| Methods | Age (Years) (Mean ± SD) | |
|---|---|---|
| CMV Antigen p65 | Positive | 0.72 ± 0.37 |
| Negative | 2.81 ± 2.03 | |
| P value | 0.3 | |
| CMV-PCR | Positive | 1.96 + 32.26 |
| Negative | 2.7 ± 2.11 | |
| P value | ˂0.001 |
Table 1. Compare the age of cases between 2 methods
| Presence of other Clinical Signs for CMV Infection | CMV-p65 |
|---|---|
| 6/17 | Positive |
| 4/18 | Negative |
| 0.4 | P value |
| CMV-PCR | |
| 5/10 | Positive |
| 4/19 | Negative |
| 1 | P value |
Table 2. Compare the variables between 2 methods
The mean age between cases with positive and negative CMV PCR was meaningful (p˂0.001) but not for CMVantigen p 65 (p=0.3).
No correlation between positive CMV results (both methods) and positive clinical signs for CMV infection (except SNHL) were observed (p=0.4, 1).
Comparison the positive CMV results between PCR and Ag-P65 methods showed significant difference between 2 methods in studied cases (Table 3).
| Variable | CMV-PCR | ||
|---|---|---|---|
| Positive | Negative | ||
| 65% | Positive | 7 | 10 |
| Negative | 2 | 19 | |
| Comparison of the CMV infection by CMV antigen and PCR | |||
| Fisher Exact test: 0.05; Actual agreement: 68.42%; KAPPA statistic: 0.33 (poor agreement); Sensitivity: 43%; Specificity: 54%; Positive predictive value: 77%; Negative predictive value: 65% | |||
Table 3. Compare the positive CMV results between PCR and AgP65 methods.
A poor agreement was seen between 2 methods for CMV infection in studied cases. Sensitivity and Specificity, PPV and NPV for CMV antigenemia (p65) in compare with positive CMV DNA (PCR) in perilymphatic fluid was 43%, 54%, 77% and 65%, respectively.
Discussion
CMV is the most common cause of congenital infection in Iran; SNHL is one of the most frequent manifestations in patients with congenital cytomegalovirus (CMV) infection [10-13]. Some authors explained the combination of serology tests for CMV-specific IgM, IgG and IgG avidity provide improved distinction between primary and secondary maternal infections [15].
In present study we observed a poor agreement between 2 methods. Positive CMV-DNA found in 26.7% (perilymphatic fluid, end organ) in compare with 43% positive CMV p65 antigenemia. Although CMV antigenemia in cases could not show the cause and effect for CMV induced SNHL, it emphasized that detection of CMV DNA is a better test for confirmation of CMV infection in end organ (perilymohatic fluid). Indeed, 77% PPV for antigenic test showed that 33% of true CMV infected cases (end organ infection) will finally be missed. The NPV (65%) determined that 35% of SNHL cases with true CMV infection might have negative antigenic test.
In the other hand, the mean age of cases with positive CMV DNA (PCR) in perilymphatic fluid was different from negative cases, but not for cases with positive antigenic tests. Indeed, mean age of cases with positive CMV DNA was higher than cases with positive antigenemia.
In our opinion, due to low sensitivity (43%) and specificity (54%) for CMV antigenemia, this test should not be used instead of CMV DNA (PCR); therefore evaluation of CMV PCR in blood and especially in end organ (perilymphatic fluid) should be measured for confirmation of CMV infection in suspected cases.
Finally, we concluded near 43% of our infants were infected with CMV (positive antigenemia) in earlier age (<1 year) but up to 27% of them would be deaf due to end organ (cochlear) damage. It confirms the causative role of CMV in producing profound SNHL in our young population. Symptomatic and asymptomatic CMV infections are a major cause of hearing loss in childhood.
Present findings are very close to previous study in Tehran, but older children with cochlear implant surgery. Of 119 children with SNHL) 16.7% [3/18] had CMV DNA in the perilymphatic fluid. Recent CMV infection (positive IgM) in 23% of cases vs. 3.3% controls); and previous immunity (positive IgG) in 51% of cases vs. 90% controls were found [11]. Here, we found higher CMV positive cases (26.7%) due to younger cases (mean age: 0.72+0.37 years) which is 2 times more than 16.7% in older cases (3-168 months) in previous study in Tehran [11]. Like here, Dollard et al. [2] reported SNHL in 14, 1% of the group with congenital CMV [2]. Also, Yamamoto et al. [6] screened 12195 infants, 121 (1%) were infected with CMV and 12 (10%) had symptomatic infection at birth. SNHL observed in 10/102 (9.8%; 95% confidence interval: 5.1-16.7) children. Profound hearing loss (>90 dB) was found in 4/5 children with bilateral SNHL while all 5 children with unilateral loss had moderate to severe deficit. The presence of symptomatic infection at birth (odds ratio, 38.1; 95% confidence interval: 1.6-916.7) was independently associated with SNHL after adjusting for intrauterine growth restriction, gestational age, gravidity and maternal age. Among 10 infants with SNHL, 6 (60%) were born to mothers with non-primary CMV infection. They concluded that even in populations with near universal immunity to CMV, congenital CMV infection is a significant cause of SNHL demonstrating the importance of CMV as a major cause of SNHL in children worldwide [4].
Ogawa et al. [4] analyzed the presence of CMV in the perilymphatic fluid and evaluated differences in the effect of cochlear implantation between CMV-positive and -negative groups. All cases with congenital infection using umbilical cord assay were be positive for CMVDNA by perilymphatic fluid assay. In addition, a CMVDNA- positive result was observed in one patient who had not been diagnosed with congenital infection. Sampling of perilymphatic fluid from a large population of patients with congenital SNHL caused by congenital CMV infection or of unknown etiology is required to determine the prevalence of CMV-related profound SNHL [3]. Recently, results of a longitudinal study for SNHL in children with congenital CMV Infection by Goderis et al. [5] published. SNHL detected in 63% of 23 children with a symptomatic and 8% of 256 children with an asymptomatic congenital CMV infection. Delayed-onset SNHL occurred in 10.6% of symptomatic CMV infection and in 7.8% of asymptomatic CMV. In the group with symptomatic CMV infection, 29.3% of children used some kind of hearing amplification; 1.6% in the group with asymptomatic CMV used hearing amplification.
The CMV seroprevalence 72.1% (CMV IgG and IgM) was reported among 240 pregnant women by Bagheri et al. [9] in Eastern states of Iran; 69.6% had a previous immunity; 27.9% had never been infected with CMV. The remaining six (2.5%) had recent infection (CMV-IgM+). 4 women (1.66%) had recurrent CMV infection (IgM+ and high IgG avidity) and 2 (0.84%) had primary CMV infection (IgM+ and low IgG avidity). Two CMV-IgM positive subjects were faced with preterm labor and low birth weight. Due to the small number of CMV-IgM positive pregnant women, they concluded that further studies should followup women with primary and recurrent CMV infection in the third trimester of pregnancy.
Some authors explained the combination of serology tests for CMV-specific IgM, IgG and IgG avidity provide improved distinction between primary and secondary maternal infections [15]. In pregnancies with confirmed primary maternal CMV infection, amniocentesis with CMV-PCR performed on amniotic fluid, undertaken after 21-22 weeks gestation, may determine whether maternofetal virus transmission has occurred. Ultrasound and, to a lesser extent, magnetic resonance imaging are valuable tools to assess fetal structural and growth abnormalities, although the absence of fetal abnormalities does not exclude fetal damage [15].
Screening for intrauterine infections during pregnancy or in neonates is not available in Iran [10-13]. First Siadati et al. [7] reported the CMV infection in primiparus pregnant women in Tehran. Sotoodeh et al. [8] described the CMV immunity in South of Iran. Congenital CMV infection developed in 2.6% of neonates [13]. Also CMV infection was one of the most common infectious agents in SNHL children in compare with healthy children [11,12]. These findings are close to serologic study upon SNHL children (compare with normal children) in our center [11]; which showed recent CMV infection was higher in the SNHL cases (P-value ˂0.001) but previous immunity (CMVIgG) was higher in the controls (P-value=0.001). But the results are far from other serological study (2006-2008) in 11 cases with idiopathic SNHL which results showed 100% of cases had previous immunity (positive CMVIgG) without none case with recent infection (positive, IgM) [12].
Conclusion
Symptomatic and asymptomatic congenital CMV infections are a major cause of SNHL in our young cases. Universal screening of newborns for congenital CMV and longitudinal audiometric follow-up are needed for all confirmed CMV infected cases. We prefer at least in our country to consider seropositive (Recent; CMV-IgM positive) SNHL children (<1 year old) as congenital form. We recommend a complete DNA assay in blood for CMV infection to differentiate between congenital and acquired infection in seropositive (CMV-IgM positive) cases after first birth day. When CMV infection is diagnosed in neonates, treatment with intravenous ganciclovir is recommended and is associated with diminished occurrence of SNHL. Oral valganciclovir for Six months also improves hearing and neurodevelopmental outcomes.
Acknowledgement
This study was supported by the Research Center of Pediatric Infectious Diseases, Iran University of Medical Sciences.
References
- Kenneson A, Cannon MJ. Review and meta-analysis of the epidemiology of congenital cytomegalovirus (CMV) infection. Rev Med Virol 2007; 17: 253-276.
- Dollard SC, Grosse SD, Ross DS. New estimates of the prevalence of neurological and sensory sequelae and mortality associated with congenital cytomegalovirus infection. Rev Med Virol 2007; 17: 355-363.
- Cannon MJ. Congenital cytomegalovirus (CMV) epidemiology and awareness. J Clin Virol 2009; 46S: S6-10.
- Ogawa H, Matsui T, Baba Y, et al. Presence of cytomegalovirus in the perilymphatic fluid of patients with profound Sensorineural hearing loss caused by congenital cytomegalovirus infection. Acta Oto-Laryngologica 2016: 136: 132-135.
- Goderis J, Keymeulen A, Smets K, et al. Hearing in children with congenital cytomegalovirus infection: Results of a longitudinal study. J Pediatr 2016; 172: 110-115e2.
- Yamamoto AY, Mussi-Pinhata MM, Isaac Mde L, et al. Congenital cytomegalovirus infection as a cause of sensorineural hearing loss in a highly immune population. Pediatr Infect Dis J 2011; 30: 1043-1046.
- Siadati A, Noorbakhsh S. CMV infection in primiparus pregnant women in Tehran. Acta Medica Iranica 2002; 40: 136-139.
- Sotoodeh A, Jamshidi M, Farjam MR, et al. Cytomegalovirus immunity in South of Iran. Am J Infect Dis 2010; 6: 8-12.
- Bagheri L, Mokhtarian H, Sarshar N, et al. Seroprevalence of cytomegalovirus infection among pregnant women in Eastern Iran. Braz J Infect Dis 2012; 16:402-403.
- Noorbakhsh S, Farhadi M, Siadati A, et al. Study of TORCH suspected infants. Iranian J Pediatr 2005; 15: 87.
- Noorbakhsh S, Farhadi M, Daneshi A, et al. Viral infections detected by serology and PCR of perilymphatic fluid in children with idiopathic sensorineural hearing loss. East Mediterranean Health Journal 2011; 17: 867-870.
- Samileh N, Ahmad S, Mohammad F, et al. Role of cytomegalovirus in sensorineural hearing loss of children: A case-control study. Tehran, Iran. Int J Pediatr Otorhinolaryngol 2008; 72: 203-208.
- Noorbakhsh S, Farhadi M, Tabatabaei A. Cytomegalovirus a common cause of intrauterine infection: A case-control study. Iran J Clin Infect Dis 2010; 5: 9-13.
- Scott HJ, Kimberlin DW. Advances in the prevention and treatment of congenital cytomegalovirus infection Curr Opin Pediatr 2016; 28: 81-85.
- Naing ZW, Scott GM, Shand A, et al. Congenital cytomegalovirus infection in pregnancy: A review of prevalence, clinical features, diagnosis and prevention. Aust N Z J Obstet Gynaecol 2016; 56: 9-18.