Current Pediatric Research
International Journal of Pediatrics
Retinopathy of prematurity: Nurses perspectives.
Bindu K. Sankar1*, Hrishikesh Amin2, Pappa. P1, Riaz M1, Shalu Varghese3
1Department of Ophthalmology, Government Nursing College, Thrissur, India
2Department of Ophthalmology, K S Hegde Medical Academy, Mangalore, India
3Department of Ophthalmology, Kerala University of Health Sciences (KUHS), Thrissur, India
- Corresponding Author:
- Bindu K. Sankar
Department of Ophthalmology,
Government Nursing College,
Thrissur,
India Thrissur,
India
E-mail: bindu.k.sankar@gmail.com
Received: 28 September, 2020, Manuscript No. AAJCP-24-19774; Editor assigned: 01 October, 2020, Pre QC No. AAJCP-24-19774 (PQ); Reviewed: 15 October, 2020, QC No. AAJCP-24-19774; Revised: 01 November, 2024, Manuscript No. AAJCP-24-19774 (R); Published: 29 November, 2024, DOI: 10.35841/0971-9032.28.11.2402-23407.
Retinopathy of Prematurity (ROP) is a leading cause of childhood blindness. India and other middle income countries are currently facing the’ third epidemic ‘of this disease mainly due to increased survival of preterm babies. This is a disorder of the immature retina of preterm babies in which abnormal vascularization occurs after birth. ROP is multifactorial; and is sensitive to the quality of neonatal inpatient care received during early life of these babies. Nurses, being the primary care givers in neonatal intensive care units, play a vital role in prevention and management of ROP.
Keywords
Retinopathy, Prematurity, Childhood blindness, Preterm babies.
Introduction
Each year approximately 15 million preterm babies are born worldwide and India has the highest number of preterm births. In 2010, it was estimated that 3,519,100 babies born preterm in India. Due to advances in neonatal care, the survival rate of these preterm babies are increasing but unfortunately all babies born preterm are vulnerable for serious health problems. Retinopathy of Prematurity (ROP) is a potentially blinding vasoproliferative disorder of the retina occurring predominantly in premature infants. It is an emerging cause of childhood blindness and can have enormous impact on the quality of life of affected infants. This is a preventable disease with a wide spectrum, either regress spontaneously or progress to severe retinal detachment leading to irreversible blindness. Nearly 50,000 infants become blind from ROP each year globally. There are approximately 1.26 million blind children worldwide and among these 280,000 children are from India. ‘Vision 2020: The right to sight’ is a global initiative launched by World Health Organization and International Agency for the Prevention of Blindness (IAPB) to eliminate avoidable blindness by the year 2020 and prevention of blindness in children is given a high priority in this program.
Literature Review
ROP, previously known as retrolental fibroplasia, was first recognized in 1942 by Dr. Theodore. L. Terry. Visual impairment from ROP has been described in three epidemics. The first epidemic of ROP occurred due to unrestricted use of oxygen. The second epidemic was reported in high income countries because of increased survival rate of very preterm babies. ROP was reported in India over a decade ago and at present, India is facing the “third epidemic” of ROP with an incidence between 38% and 51.9% which varies considerably in different states of the country. This is because of many reasons, the major being the increased survival rate of preterm infants, inadequate and suboptimal care provided in Neonatal Intensive Care Units (NICUs) and low coverage of services for screening and treatment for ROP.
How does ROP develop?
The eye starts to develop at about 16 weeks of gestation and the formation of retinal blood vessels begin at the optic nerve in the back of the eye and progress gradually towards the edges of the retina supplying oxygen and nutrients. Rapid development occurs during the last 12 weeks of pregnancy. But when a baby is born preterm, must develop in a suboptimal environment. Normal blood vessel growth may stop before these vessels reach the edges of retina. So abnormal new blood vessels start to grow and spread throughout retina. As these abnormal vessels are very fragile and leak easily, they scar the retina and pull it out of its normal position. This leads to retinal detachment which is the major cause of visual impairment and blindness in ROP.
Discussion
Classification of ROP
International Classification of ROP (ICROP) was published in 1984 to standardize terminologies used to describe ROP. It was later revised in 2005.This classification explains
• The severity or stages of ROP
• The location or zone of the disease
• Extent of the disease
• Presence or absence of plus disease
• Presence or absence of aggressive posterior ROP
Severity (stages) of ROP
ROP can develop when the immature retinal blood vessels have not reached the edge of the retina (ora serrate) and may progress slowly or rapidly.
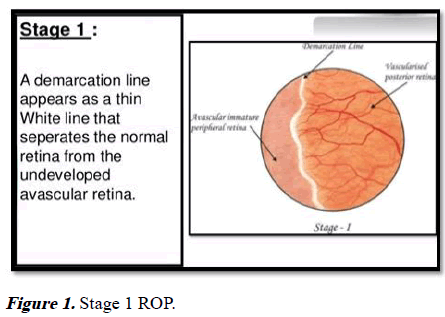
Stage 1 ROP: Characterized by demarcation line. A whitish line is visible between the normally vascularised retina and the peripheral retina in which there are no blood vessels.
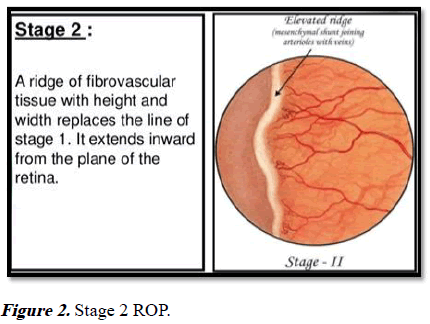
Stage 2 ROP: Visible ridge. The demarcation line develops into a ridge with height and width, between the vascular retina and peripheral retina.
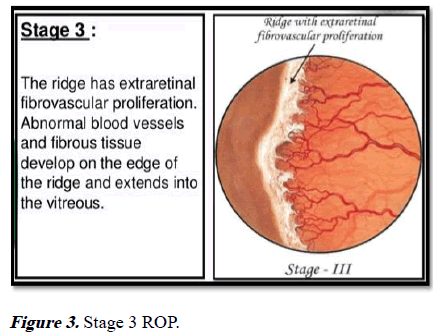
Stage 3 ROP: Blood vessels in the ridge. Blood vessels grow and multiply (proliferate) and are visible in the ridge.
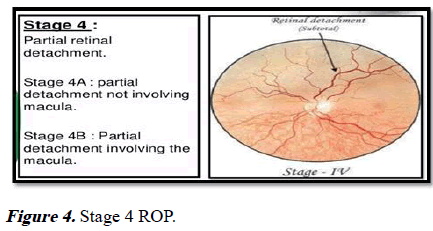
Stage 4 ROP: Sub-total/partial retinal detachment. It occurs due to anterior pulling of the retina by the scar tissue into the vitreous. Depending on the extent of involvement stage 4 is further divided in to stage 4A (macula is not involved) and stage 4B (macula is involved).
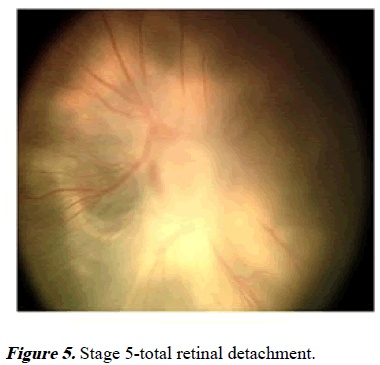
Stage 5 ROP: Total retinal detachment.
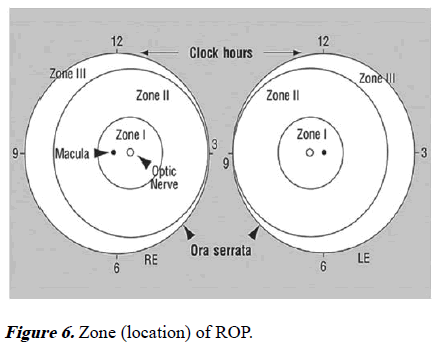
Location of disease
The development of normal blood vessels in retina is from the optic nerve posteriorly to ora serrate anteriorly.
Zone I: A small circle with a radius of twice the distance from the macula to the centre of optic disc. Disease involving zone 1 is considered as most serious.
Zone II: Area of retina surrounding zone I. A circle with a radius of distance from centre of optic disc to the nasal margin of retina.
Zone III: Area of retina from zone II to ora serrate on nasal side and equator on temporal side.
Extent of disease
The retina is divided in to 12 sectors similar to a clock and the number of clock hours of the eye’s circumference involved is defined as the extent of ROP.
Plus disease: It is characterized by dilatation and tortuosity of retinal arterioles and venules near the optic disc.
Pre threshold ROP: This is defined as the presence of less than threshold disease in zone I or stage 2 plus disease in zone II or stage 3 without plus disease in zone II or stage 3 plus disease with extent less than that for threshold disease.
Threshold ROP: This is defined as zone I or zone II with stage 3+ROP extending for 5 contiguous sectors or 8 composite sectors.
Aggressive posterior ROP: This is a rare, but rapidly progressing, severe form of ROP. It was previously referred to as “rush disease”. This type of ROP is posteriorly located, with prominent plus disease and nearly always in zone II. AP-ROP should be recognized and treated within 48 hours as it can progress rapidly to retinal detachment.
In December 2003, a new clinical algorithm was produced following the Early Treatment of ROP (ETROP) study funded by National Eye Institute, United States of America. As per this: Type 1: Zone I with any stage with plus disease, zone I with stage 3 without plus disease and zone II with stage 2 or 3 with plus disease. Type 2: Zone I with stage1 or 2 without plus disease, zone II with stage 3 without plus disease.
Role of nurses in prevention and management of ROP
Prevention of blindness related to ROP need a multidisciplinary team approach. The team consists of obstetricians, neonatologists, ophthalmologists, nurses, paediatricians, health care workers and parents. In addition to prematurity and low birth weight, many studies report other risk factors for development of this disease such as oxygen therapy, mechanical ventilation, sepsis, respiratory distress, blood transfusion, poor weight gain and anemia. Preterm babies are not born with ROP, but develop this during the course of their NICU stay most of the time. Neonatal nurses are pillars of the neonatal intensive care units and ROP is sensitive to the quality of neonatal inpatient care especially nursing care. Nurses with adequate knowledge and skills are essential in providing best practices for prevention of ROP. They act as primary caregivers, client advocate, nurse leaders and counsellors for the family. As a member of comprehensive child services team nurses are involved in all the three levels of prevention of this potentially blinding disorder. Nurses working in community can also contribute significantly.
Primary prevention
Primary prevention of ROP include strategies to reduce the rate of premature birth by improving antenatal care and quality of neonatal care. India is a developing country and majority of people live in rural areas. They have minimum access and availability of health care facilities. Community health workers especially nurses and ASHA workers play an important role in providing cost-effective interventions for a healthy pregnancy and better outcome.
A significant proportion of preterm babies (who born between >20 and <37 weeks of gestation) experience lifelong disabilities and health issues. So the rate of preterm births to be reduced to a minimum and nurses working in hospitals as well as in community can involve in following:
Creating public awareness to prevent preterm births by controlling biological, clinical and socio-behavioral risk factors. Education should focus on:
• Measures to avoid teenage pregnancies
• Maintain adequate pre pregnancy body weight
• Iron and folic acid supplementation
• Control and proper management of chronic diseases
• Cessation of harmful health habits eg smoking, alcoholism,
substance abuse
• Judicious use of infertility treatment
• Improve mental health
• Proper screening and management of high risk pregnancies
• Special care in pregnancies with bad obstetrical histories
eg. Cervical encirclage, use of vaginal progesterone
• Use of antenatal steroid in women with preterm labour
before 34 weeks and also in cases of premature rupture of
membrane under 32 weeks’ gestation.
Care of preterm delivery-care during “Golden hour” to maximise survival and minimise morbidity.
• Prevention of hypothermia in labour room
• Avoid initial 100% oxygen administration and preferable
use of nasal CPAP rather than mechanical or manual
ventilation
Safe and standard practices in NICU which can be summarised as POINTS of care. (P-pain control, O-judicious use of Oxygen, I-infection control measures, N-adequate nutrition, Tthermoregulation, S-supportive care.)
• Pain increases the babies’ need for oxygen and worsen
respiratory distress. It makes the babies unstable. Avoid
unnecessary painful procedures, anticipate pain and take pain relieving measures such as oral glucose/sucrose or
swaddling during procedures.
• Oxygen supplementation. Ensure that oxygen saturation is
between 89%-94% and set alarms accordingly. Use of
blenders and CPAP are preferable.
• Practice infection control measures strictly. Neonatal
infections, especially fungal infections are also risk factors
for ROP.
• Provide adequate nutrition and monitor weight gain. Use
breast milk as far as possible but supplement extra calories
and proteins. Post-natal weight gain predicts the risk of
ROP.
• Thermoregulation. Prevention of hypothermia is of utmost
importance and kangaroo mother care can be promoted to
keep the baby warm, to increase maternal breast milk
production as well as to improve child parent bonding. Use
a plastic bag or occlusive wrapping to prevent heat loss.
• Supportive developmental care for normal neuromuscular
development. Reduce the stress of preterm babies as this
can lead to fluctuations in oxygen saturation. Minimise
bright lights and sounds in NICU. Position babies
comfortably with their limbs supported. Minimal handling
of the babies and clustering of nursing procedures are
recommended as these will provide adequate periods of
uninterrupted sleep.
• Avoid blood transfusions as far as possible.
• Prevention of anaemia. Delayed cord clamping is advised.
In premature new-borns, anaemia is often exacerbated by
withdrawing too much blood for lab tests too often.
• Standard neonatal care practises, good infrastructure and
availability of resources also need attention. Pulse
oximeters, oxygen blenders and CPAP units should be
available in sufficient number.
• Regular training, workshops and conferences should be
conducted for obstetricians, neonatologists and nurses to
update their knowledge and skill for providing safe and
standard neonatal care.
Secondary prevention
Secondary prevention includes screening and treatment of ROP. This disease is asymptomatic in its early course and starts only two three weeks after birth thus providing adequate time for early detection and treatment.
Screening guidelines
Screening guidelines vary across different countries and even different centers. The latest ROP screening guidelines published by the American Academy of Paediatrics and American Academy of Ophthalmology (AAP/AAO) recommend screening of all infants with gestational age of less than or equal to 30 weeks and/or birth weight less than or equal to 1500 g or with unstable clinical course as per the treating neonatologist’s suggestion.
Latest Indian screening guidelines:
• Birth weight <1700 g
• Gestational age of <34-35 weeks at birth
• Received oxygen supplementation >30 days
• Infants born at <28 weeks and weighing <1200 g are
particularly at high risk of developing severe form of ROP
• The presence of other factors such as respiratory distress
syndrome, sepsis, multiple blood transfusions, multiple
births (twins/triplets), apnoea and intraventricular
haemorrhage increase risk of ROP. In these cases, screening
should be considered even for babies >37 weeks’ gestation
or >1700 g birth weight.
In India, it is seen babies falling outside the above mentioned criteria also develop sight-threatening ROP due to the variation in quality of neonatal care across the country. So the guidelines were revised and now it is recommended to screen all babies with birth weight <2000 gm or gestational age <34 weeks or infants with unstable clinical course who are at risk as per neonatologist. To avoid confusions about the timing of first screening Jalali et al recommend “day 30 day 20” strategy i.e., first ROP screening should be done strictly before “day 30” of post-natal life and by “day 20” of life in smaller babies. (<30 weeks and/or birth weight <1200 g). Better compliance is seen with this day 30 day 20 strategy as it is easy to remember the date of birth of these babies by all health care providers. Screening is performed by an expert using indirect ophthalmoscopy.
Role of nurses in ROP screening
Screening
• Record weight and gestational age at birth
• Monitor weight gain during NICU admission
• Select babies eligible for screening
• Counsel the parents regarding screening procedure
• Dilate eyes one hour before examination using a topical
agent
• Keep the baby nil per oral one hour prior to procedure
• Position the baby comfortably, take adequate pain control
measures
• Ensure hand washing, use sterile articles only during
procedure
• Monitor vital signs
• Documentation of procedure, fix next appointment
Treatment
ROP can advance rapidly and any delay in treatment will reduce the chances of success. So it should be cosidered as a medical emergency and treatment is warranted within 48 hours of diagnosis in severe form and as soon as possible in APROP. Cryotherapy was the initial treatment modality, but less frequently used now a day. Currently, laser photocoagulation in which ablating the peripheral avascular retina, is the treatment of choice because of more precision and less unfavourable side effects. Adequate and timely laser treatment has a success rate of around 90%. In case of severe ROP and those who do not respond to laser photocoagulation, anti-VEGF (Vascular Endothelial Growth Factor) is also used. But it is not used as first line therapy. There are controversies regarding long term complications of this on eye as well as systemic complications like developmental delay. Use of propanalol, treatment with IGF-1,vitamin E and gene therapy are also under investigation for the treatment of this disease. Surgical interventions such as scleral buckling, lens sparing vitrectomy, lensectomy with vitrectomy or open sky vitrectomy may be needed to treat stage 4 and 5 of ROP and these procedures are performed only by paediatric retinal surgeons.
Awareness of ROP among parents
ROP screening may require multiple visits even after discharge from NICU. Noncompliance and failure to follow up regularly are the most common challenges in ROP screening. Parents need to be made aware of the disease process and the importance of frequent follow up so that adverse events can be prevented. Rapid progression of disease and need for early intervention such as laser should be communicated to parents. Nurses in NICU can play a major role in counselling the parents as they have frequent interaction with them. Ophthalmologists should reassure the parents that laser treatment will not cause any harm to their child. Accredited Social Health Activist (ASHA) workers in rural area can also play a pivotal role in counselling the parents during their home visits. Public awareness also should be raised through print and electronic media and by placing hoardings by celebrities regarding ROP.
Barriers for secondary prevention
A developing country like India face many challenges for the effective implementation of screening and treatment strategies. Of course, the escalation and standardization of neonatal care have led to better survival of preterm babies, but availability of ROP screening and treatment is not in pace with that which in turn lead to increased visual morbidity due to ROP. Recent studies report that awareness among paediatricians about ROP is poor and babies are referred to ophthalmologists for ROP screening too late when they notice a white reflex or the parents complaint of the same. By the time the baby may be irreversibly blind. Non availability of trained personnel, ignorance of parents and health care personnel, distance of point of care, lack of adequate infrastructure such as indirect ophthalmoscope for screening and laser machines for treatment of ROP are the main existing barriers causing delay, There are only <200 ROP specialists nationwide which act as a major hindrance for timely screening. So more and more ophthalmologists must be trained in ROP screening and management. Regular medical education programs and workshops on ROP should be conducted to expertise ophthalmologists, neonatologists and paediatricians and a better rapport must be established between them. ROP should be given due importance in the curriculum of doctors and nurses in all levels. In case of non-availability of trained ophthalmologists, tele screening is another option and recent studies show that nurses and other non-physicians can be trained successfully in tele screening and utilize them in areas where trained ophthalmologists are not available.
Tertiary prevention
Long term visual rehabilitation is the key to achieving optimal visual outcomes. Tertiary prevention includes treating complications to prevent visual disabilities or improve visual function by correction of refractive errors. Many of these children need to wear spectacles from early childhood and repeated counselling of parents may be necessary. Lack of screening is the most common reason for stage 5 ROP in India. If all preterm babies at risk are screened on time we can prevent stage 4 or 5 ROP from occurring which will reduce the chance for visual disabilities. Sometimes, even after laser treatment disease progresses to stage 4 or 5. Resolution of treated ROP may end up with vision impairing ocular morbidities such as refractive errors especially high myopia, strabismus, amblyopia, cataract, glaucoma and cortical visual impairment. It may become necessary to have long term follow up by paediatric ophthalmologists regarding which parents need to be informed. Good vision from early infancy is critically essential for normal child development as vision coordinate other sensory inputs and help the child to understand his environment and develop psychomotor and cognitive function. Visual rehabilitation of the affected children is also important. They need to be helped to achieve physical, social, emotional and spiritual independence and optimum quality of life. Blind children should receive special education and trained for leading a productive life. Parental and social support are of utmost important in bringing up these children. Rehabilitation services of these children should be integrated into the health system to ensure the continuity of care.
Future plan of action
International standards for neonatal care should be established globally to foster better survival and neonatal outcomes. There is a potential for developing a cadre of specialist ROP nurses, but unfortunately there are very few formal training programs for neonatal nurses in our country. Competency based training should be conducted emphasizing the role of nurses in prevention and management of ROP. Accreditation for neonatal nurses as a specialist will provide opportunities for career development and better understanding of multiple dimensions of their roles. For making a sustainable change, leadership from within the nursing profession should come up and experienced neonatal nurses can mentor the junior staff to improve quality of care in NICU14. Nurses can be trained for ROP screening and there are research findings which showed nurses are capable to perform ROP screening as it is carried out by an expert pediatric ophthalmologist. This can be practised in tertiary care settings as a specialised area for developing nursing leadership in prevention of ROP. Nurses in community also can be prepared for telescreening and may be utilized for bridging the gap whenever experts are not available especially in rural areas.
Conclusion
It is very difficult to predict or control premature birth, but high quality neonatal care, timely screening and treatment of ROP can reduce the number of infants becoming blind or visually impaired. Realizing its importance, ROP is included in new-born screening program under Rashtriya Bal Swasthya Karyakram (RBSK) by the Government of India. Competencybased training of medical professionals including neonatologists paediatricians, ophthalmologists and nurses should be conducted regularly. Nurses, being the primary care givers in NICU can advocate for providing standard practices which in turn lead to optimal neuro developmental outcomes. Creating awareness regarding ROP among the public and all the stakeholders involved in care of preterm babies is essential to prevent avoidable visual impairment. Forget about all egos and politics, work as a team of neonatologists, nursing staff and ophthalmologists for healthy survival of preterm infants.
References
- Radhakrishnan N, Pillai GS, Kiran KR, et al. Retinopathy of prematurity-an overview. Kerala J Ophthalmol 2017; 29: 154-159.
- Goyal A, Giridhar A, Gopalakrishnan M. Real-world scenario of retinopathy of prematurity in Kerala. Kerala J Ophthalmol 2017; 29: 30-34.
- Akkawi MT, Shehadeh MM, Shams AN, et al. Incidence and risk factors of retinopathy of prematurity in three neonatal intensive care units in palestine. BMC Ophthalmol 2019; 19: 1-7.
[Crossref] [Google Scholar] [PubMed]
- Vinekar A, Dogra M, Azad RV, et al. The changing scenario of retinopathy of prematurity in middle and low income countries: Unique solutions for unique problems. Indian J Ophthalmol 2019; 67: 717-719.
[Crossref] [Google Scholar] [PubMed]
- Vinekar A, Dogra MR, Sangtam T, et al. Retinopathy of prematurity in Asian Indian babies weighing greater than 1250 grams at birth: Ten year data from a tertiary care center in a developing country. Indian J Ophthalmol 2007; 55: 331-336.
[Crossref] [Google Scholar] [PubMed]
- Coe K. Nursing update on retinopathy of prematurity. J Obstet Gynecol Neonatal Nurs 2007; 36: 288-292.
[Crossref] [Google Scholar] [PubMed]
- Darlow BA, Gilbert CE, Quiroga AM. Setting up and improving retinopathy of prematurity programs: Interaction of neonatology, nursing and ophthalmology. Clin Perinatol 2013; 40: 215-227.
[Crossref] [Google Scholar] [PubMed]
- Karkhaneh R, Mousavi SZ, Riazi-Esfahani M, et al. Incidence and risk factors of retinopathy of prematurity in a tertiary eye hospital in Tehran. Br J Ophthalmol 2008; 92: 1446-1449.
[Crossref] [Google Scholar] [PubMed]
- Kalyan GE, Moxon S. The role of neonatal nurses in the prevention of retinopathy of prematurity. Indian Pediatr 2016; 53: S143-S150.
[Google Scholar] [PubMed]
- Kiranmayee PS, Kalluri V. India to gear up to the challenge of “third epidemic” of retinopathy of prematurity in the world. Indian J Ophthalmol 2019; 67: 726-731.
[Crossref] [Google Scholar] [PubMed]