Current Pediatric Research
International Journal of Pediatrics
Postpartum hemorrhage and associated factors among mothers who delivered at public health institutions in Ethiopia: A systematic review and meta-analysis.
Yoseph Merkeb Alamneh*, Fentahun Adane
Department of Biomedical Science, Debre Markos University, Debre Markos, Ethiopia
- Corresponding Author:
- Yoseph Merkeb Alamneh
Department of Biomedical Science,
Debre Markos University,
Debre Markos,
Ethiopia
E-mail: ymerkeb11@gmail.com
Received: 27 February, 2024, Manuscript No. AAJCP-20-18132; Editor assigned: 01 March, 2024, Pre QC No. AAJCP-20-18132 (PQ); Reviewed: 15 March, 2024, QC No. AAJCP-20-18132; Revised: 22 March, 2024, Manuscript No. AAJCP-20-18132 (R); Published: 29 March, 2024, DOI:10.35841/0971-9032.28.03.2184-2188.
Background: Despite postpartum hemorrhage is a preventable and manageable condition; it remains the leading cause of maternal morbidity and mortality worldwide. In Ethiopia, there is a scarcity and high variability of information regarding the magnitude and associated factors of postpartum hemorrhage. Thus, this study was aimed to assess the pooled prevalence and associated factors of postpartum hemorrhage among mothers at public health institutions in Ethiopia. Methods: The universal databases include MEDLINE/PubMed, EMBASE, Scopus, and Grey literature databases, Google Scholar, Science Direct and Cochrane library were extensively searched. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) 2009 guidelines have pursued this review. STATA version 14 with 95% CI was used to analyze the data and I2 test was used to assess the heterogeneity between the studies. Egger's test was used to assess publication bias. The quality of each study was assessed using the Newcastle- Ottawa quality assessment tool and metaanalysis was conducted using a random-effects model. Result: Eleven studies with a total of 16, 416 delivered women were included in this meta-analysis. The pooled national level prevalence of postpartum hemorrhage among mothers who delivered at public health institutions in Ethiopia was12.50% (95% CI: 9.4, 15.27). Mothers aged 35and above (OR: 2.40, 95% CI: 1.41-4.09), Living in rural (OR: 3.08, 95% CI: 1.52-6.25), grand multi-parity (OR: 3.73, 95% CI: 1.32-6.55), antenatal care follows up (OR: 4.82, 95% CI: 3.43-8.71), Previous history of postpartum hemorrhage (OR: 3.22, 95% CI: 2.02-5.15), cesarean section and instrumental delivery (OR: 6.67, 95% CI: 2.92-6.23) were independent risk factors. Conclusions and Recommendation: The pooled national level prevalence of postpartum hemorrhage among mothers who delivered at public health institutions in Ethiopia was relatively high despite the government launches different strategies to prevent postpartum hemorrhage. Older age, residency, grand multi-parity, antenatal care follows up, the previous history of postpartum hemorrhage and mode of delivery were the major predictor variables. Hence, appropriate intervention on potential determinates could be addressed by extra vigilance during labor and preparedness for PPH management in all women giving birth.
Keywords
Ethiopia, Magnitude, Associated factors, Postpartum hemorrhage.
Introduction
Postpartum Hemorrhage (PPH) refers to a blood loss of 500 ml or greater within 24 hours. Blood loss may occur during and after vaginal delivery but blood loss may exceed >1000 ml in the cesarean section delivery. Globally in 2017, an approximate 216 million maternal deaths were reported per 100,000 births per year, of which 90% occur in developing countries such as Ethiopia. Globally, hemorrhage is the first leading cause of maternal mortality according to WHO 2014 report. WHO 2016 report indicates that in developing countries, including Ethiopia, about 14 million mothers worldwide suffer from vaginal bleeding during or after birth; the risk of maternal mortality caused by postpartum hemorrhage is 1 in 1000 deliveries.
WHO 2015 report showed that about 99% of maternal deaths from vaginal bleeding after childbirth occurred in lowand middle-income countries. Following a decrease in maternal mortality in Ethiopia, the incidence is about as high as 412 per 100,000 live births, the most challenging problem being rising maternal mortality [1].
The incidence of PPH is a major public health concern in developing countries, including sub-Saharan African countries. The occurrence of PPH ranges between countries, for instance in Pakistan 6%, in Uganda 7.4% and in India 22.7%. Ethiopia is also one of the SSA countries with a high variability in the occurrence of PPH ranging from 1.4% to 9.69%. In Ethiopia, the associated factors of postpartum hemorrhage ranged from region to region and across various articles.
While, the government in Ethiopia launches different strategies to prevent postpartum hemorrhage, maternal mortality due to hemorrhage is still high. Despite this fact, in Ethiopia, there is a scarcity and variability of information regarding the magnitude and associated factors of postpartum hemorrhage. Thus, this study was aimed to assess the overall magnitude and associated factors of postpartum hemorrhage among mothers at public health institutions in Ethiopia.
Determining the pooled magnitude and associated factors is therefore important for policy makers and stakeholders to reduce maternal morbidity and mortality as a result of postpartum hemorrhage. The findings of this study will also be useful for researchers by serving as baseline information.
Materials and Methods
Study design and setting
This systematic review and meta-analysis was performed to assess postpartum hemorrhage severity and associated factors among mothers who delivered at Ethiopia’s public health institutions. Ethiopia is located in the horn of Africa. It is surrounded by Eritrea in the north, Djibouti in the east, Sudan and South Sudan in the west and Kenya in the south [2].
Search strategies
This systemic review and meta-analysis were considered to estimate the pooled magnitude and associated factors of postpartum hemorrhage among mothers who delivered at Ethiopian public health institutions. The protocol of this systematic review and meta-analysis has been registered on an international Prospective Register of Systematic Review (PROSPERO), university of York center for reviews and disseminations. The registration number is CRD187704. The Preferred Reporting Items for Systematic Reviews and Meta- Analysis (PRISMA) guideline was used to confirm the scientific accuracy. In this study, we searched for potentially applicable papers, such as PubMed/MEDLINE, the Science Web, EMBASE, CINAHL, HINARI, Google Scholar, Science Direct, Cochrane Library and other sources. Endnote (version X7) reference management software was used to download, organize, review and cite the articles. This review included all articles published in peer-reviewed journals that were written in the English language given that such language restriction does not alter the outcome of the systematic reviews and metaanalysis. Also, gray literature of observational studies and official websites of international and local organizations and universities were used [3]. The search of the literature was conducted from the 1st of December to December 30, 2019. All papers published until December 30, 2019, were considered. The electronic databases were searched by Medical Subject Headings (MeSH) terms and using the following keywords magnitude, prevalence, epidemiology, and delivered women, predictors determinants, associated factors, postpartum hemorrhage and Ethiopia. We used the search terms independently and/or in combination using Boolean operators like “OR” or “AND”.
Eligibility criteria
Study area: Studies conducted in Ethiopia only were
considered.
Population: All mothers who delivered in public health
institutions were the study population.
Publication condition: Both published and unpublished
articles were considered.
Study design: All observational study designs reporting the
magnitude and associated factors of postpartum hemorrhage
among mothers who delivered at public health hospitals were
considered.
Language: Articles reported only in the English language were
considered.
Data extraction and quality assessment
Data were extracted using a standardized data extraction spreadsheet format in Microsoft Excel. The data abstraction format includes author/s name, year of publication, study region, study design, sample size, the magnitude and associated factors of postpartum hemorrhage. All published and unpublished primary studies those written in the English language and conducted at Ethiopian public health institutions were included. The data were extracted by two independent authors (YM and FA). Joanna Briggs Institute (JBI's) critical appraisal checklist for prevalence studies was used to assess the quality of included studies. Additionally, a modified version of the Newcastle-Ottawa Scale (NOS) was used to assess the methodological quality of studies for cross-sectional studies. Newcastle-Ottawa scale criteria include representativeness of the sample, response rate, measurement tool used, comparability of the subject, appropriateness of the statistical test used to analyze the data. Based on the Newcastle-Ottawa scale criteria, two authors (YM and FA) independently assessed the quality of each article. Any discrepancy was resolved through discussion and consensus. Articles with medium to high quality (≥ 6 out of 10 stars) were included within this analysis [4].
Data processing and analysis
After extracting the data using Microsoft Excel format, we imported the data to statistical program STATA version 15.0 for further analysis. We identify the heterogeneity between the studies using Cochrane's Q statistics inverse variance (I2) and p-values. As the test statistic showed there is significant heterogeneity among the studies, as a result, a random-effects meta-analysis model was used to estimate the DerSimonian and Laird's pooled effect. In the current meta-analysis, arcsinetransformed proportions were used. The pooled magnitude was estimated by using the back-transform of the weighted mean of the transformed proportions, using arcsine variance weights for the fixed-effects model and DerSimonian-Laird weights for the random-effects model. Egger’s and Begg’s tests, with the p-value, less than 5% was used to declare the presence of publication bias.
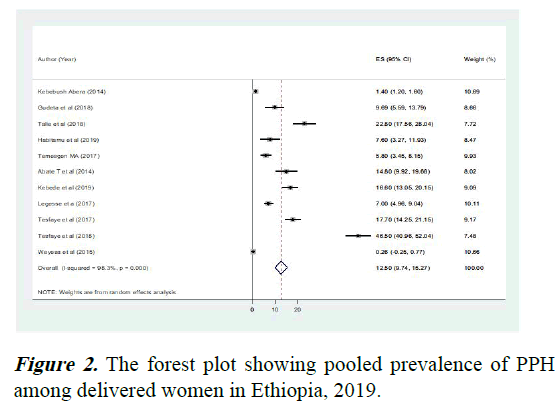
Also, using forest plot, point prevalence, as well as 95% confidence intervals, was presented. In this forest plot, the size of each box indicated the weight of the study, while each crossed line refers to a 95% confidence interval. For the second outcome, a log odds ratio was used to determine the association between determinant factors and magnitude of PPH.
Results
Study selection and data extraction
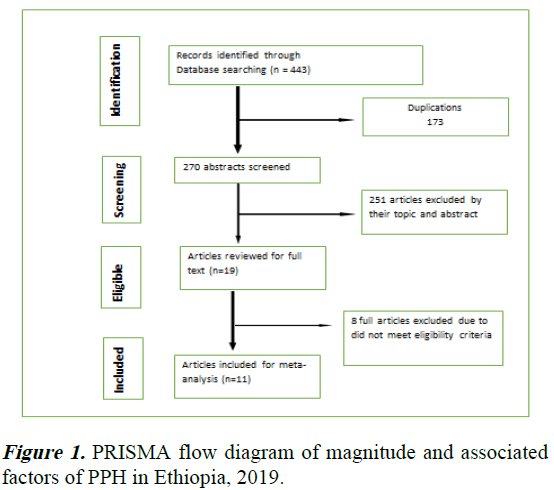
This systematic review and meta-analysis have been reported by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. Initially, 443 articles related to the magnitude and predictors of PPH were found. Of these, 173 duplications and 251 unrelated articles were excluded. Second, from the remaining 19 potential articles, 11 met eligibility for the review and included in the analysis. The rest eight full-text articles were excluded due to did not meet outcomes of interest or study area (Figure 1).
Characteristics of included studies
Ten included studies were cross-sectional and one study was case-control in study design. The total sample size used were 16,416 women to estimate the pooled prevalence of postpartum hemorrhage. All the included articles were published. The main characteristics of the included studies are described [5].
Meta-analysis
The magnitude of postpartum haemorrhage: The lowest prevalence rate of postpartum hemorrhage was 0.26% observed in a study conducted at SNNP and the highest was 46.50% observed in a study conducted at Harar.
The I2 test result showed that there was high heterogeneity with I2=98.5% at the p-value ≤ 0.001. Based on the random effect analysis, the pooled national level magnitude of PPH among women in public hospital delivery in Ethiopia was 12.50% (95% CI: 9.4, 15.27) (Figure 2) [6].
Heterogeneity and publication bias
The existence of publication bias was evaluated by visual examination of the funnel plot and Egger's test. Visual examination of the funnel plot indicated asymmetrical distribution of included studies. We also observed publication bias in magnitude of PPH using both Begg's and Egger's tests and these tests showed that there was statistical evidence of publication bias at p-value less than 0.05 and the funnel plot was asymmetry. By consideration of publication bias trim and fill meta-analysis were done. However, based on this analysis no significant change was shown as compared with the main meta-analysis. The result of this meta-analysis revealed statistically significant heterogeneity among studies, a subgroup analysis by region was computed to compare the magnitude of PPH across regions of the country. Based on subgroup analysis, the highest magnitude of PPH was observed in the Amhara region, 12.523% (95%, CI: 5.251, 19.794) followed by the SNNP region, 10.99 (95%, CI: 0.45, 21.53) [7].
Meta-regression
In addition to subgroup analysis and publication bias, univariate and categorical meta-regression analysis was performed by considering both continuous and categorical data for the included studies to identify heterogeneity sources for pooled prevalence. In the meta-regression analysis, sample size, publication year and study regions were considered for each study. However, there was no statistical significance value of the meta-regression analysis (Table 1) [8].
| Variables | Characteristics | Coefficient | P-value |
|---|---|---|---|
| Year | Publication year | 3.127061 | 0.212 |
| Sample size | Adiss Ababa | 0.0011445 | 0.342 |
| Amhara | 25.01484 | 0.193 | |
| Region | SNNP | 11.25309 | 0.394 |
Table 1. Meta-regression for the included studies to identify the source of heterogeneity for the magnitude of PPH in Ethiopia, 2019.
Associated factors of postpartum hemorrhage
In this meta-analysis, study conducted in Ethiopia had seen the relation between the magnitude of PPH and maternal-age. The meta-analysis of these studies showed that the magnitude of PPH was correlated significantly with maternal age above 35 years (OR: 2.40, 95% CI: 1.41-4.09). Specifically, the probability of PPH magnitude was 2.40 times greater for women above 35 years of age compared with their counterparts. In this study, the magnitude of PPH was found to be significantly associated with women who lived in a rural area (OR: 3.08, 95% CI: 1.52-6.25). Also, women who lived in a rural area were around three times more likely to develop PPH compared to those women who lived urban. In this analysis the risk of developing PPH increases as gravity and parity rise. The meta-analysis of these studies showed that the magnitude of PPH was correlated significantly with women who were grand multiparous (OR: 3.73, 95% CI: 1.32-6.55). This review revealed that the magnitude of PPH was high in women who had no ANC follow up when compared with mothers who had ANC follow up (OR: 4.82, 95% CI: 3.43-8.71). This review also identified that a previous history of PPH was another variable which significantly associated with the magnitude of PPH (OR: 3.22, 95% CI: 2.02-5.15). Finally, women who delivered by instrumental and cesarean section were about four times more likely to develop PPH compared to those who delivered spontaneously vaginally (OR: 3.67, 95% CI: 2.92-6.23) [9].
Discussion
This systematic review and meta-analysis, as we know, is first to estimate the pooled prevalence of PPH among women who delivered at the Ethiopian public health institution. In addition, the determinant factors influencing the magnitude of PPH were also seen. According to this systematic review and metaanalysis, the pooled approximate prevalence of PPH among women who delivered at Ethiopia’s public health institution was 12.50% (95% CI: 9.4, 15.27). The overall magnitude of this study is consistent with results from previous studies in sub-Saharan Africa countries with a prevalence of 10.5% and Tanzania with a total prevalence of 11.9%. However, the finding of the present study was higher as compared to the studies done in other countries such as Australia 4.4%, Uganda 9%, globally 6%. On the other hand, this finding was lower than the results of the studies done in Pakistan with a prevalence of 21.3% and Cameron with the magnitude of 23%. The possible reason for this may be due to the study area and study setting, prenatal, postnatal care, sample size disparity, socio-cultural and socio-demographic, methodological and study time across those countries that result in differences in prevalence levels in the above-mentioned studies compared to this study. Additionally, this variation between the studies may have been influenced by the characteristics of the study population; those were rural women that are reported to have higher rates of PPH. The magnitude of PPH was varied across regions in Ethiopia. Based on subgroup analysis, the highest magnitude of PPH was observed in the Amhara region followed by the SNNP region. This may be due to methodological, sociocultural and socio-demographic, methodological and time of the study difference across regions [10].
The meta-analysis of these studies revealed that as the mother’s age increases the risk of experiencing PPH was increased. This result was supported by similar findings, which revealed that mothers aged 35 or above were more likely to experience PPH, from the studies done in France, Uganda and Pakistan. This may be because myometry function deteriorates with age in older people, uterine atony is the most common cause of postpartum hemorrhage, pre-existing medical conditions such as diabetes mellitus or hypertension and placenta praevia is an independent risk factor for PPH. This review also identified that mothers with a history of previous postpartum hemorrhage were found around three times more risk of postpartum hemorrhage than those with no history PPH. This finding was supported by the studies done in Cameroon and Norway. The reason for this may be a previous PPH can predict subsequent risk of hemorrhage
Conclusion
The pooled national level prevalence of postpartum hemorrhage among mothers who delivered at Ethiopia’s public health institutions was relatively high despite the government launches different strategies to prevent postpartum hemorrhage. Older age, residency, grand multi-parity, antenatal care follows up, the previous history of postpartum hemorrhage and mode of delivery were the major predictor variables. Hence, appropriate intervention on potential determinates could be addressed by extra vigilance during labor and preparedness for PPH management in all women giving birth.
Limitations
The results of this systematic review and meta-analysis had limitations: Primarily, this systematic review and meta-analysis used internationally accepted tools for critical appraisal system for quality assessment of individual studies.
Secondly, since the studies were conducted only on the five regions which reduce its representativeness for the country and cross-sectional unable to show a causal relationship.
Availability of Data and Material
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
Competing Interests
We have confirmed that we have no competing interests.
Funding
No funding was obtained for this study.
Acknowledgment
We gratefully thank the primary authors of the included studies.
References
- Bai J, Sun Q, Zhai H. A comparison of oxytocin and carboprost tromethamine in the prevention of postpartum hemorrhage in high‑risk patients undergoing cesarean delivery. Exp Ther Med 2014; 7: 46-50.
[Crossref] [Google Scholar] [PubMed]
- Tessema GA, Laurence CO, Melaku YA, et al. Trends and causes of maternal mortality in Ethiopia during 1990-2013: Findings from the global burden of diseases study 2013. BMC Public Health 2017; 17: 1-8.
[Crossref] [Google Scholar] [PubMed]
- Bhat PB, Navada MH, Rao SV, et al. Evaluation of obstetric admissions to intensive care unit of a tertiary referral center in coastal India. Indian J Criti Care Med 2013; 17: 34.
[Crossref] [Google Scholar] [PubMed]
- Habitamu D, Goshu YA, Zeleke LB. The magnitude and associated factors of postpartum hemorrhage among mothers who delivered at Debre Tabor general hospital 2018. BMC Res Note 2019; 12: 1-6.
[Crossref] [Google Scholar] [PubMed]
- Moher D, Pham B, Lawson ML, et al. The inclusion of reports of randomised trials published in languages other than English in systematic reviews. Health Technol Assess 2003; 7: 1-90.
[Crossref] [Google Scholar] [PubMed]
- Amanuel T, Dache A, Dona A. Postpartum hemorrhage and its associated factors among women who gave birth at Yirgalem general hospital, Sidama regional state, Ethiopia. Health Serv Res Manag Epidemiol 2021; 8: 23333928211062777.
[Crossref] [Google Scholar] [PubMed]
- Zenebe GA, Zenebe WA, Ewunie TM, et al. Primary postpartum hemorrhage and associated factors among delivering women in Gedeo zone, Southern Ethiopia. Front Med 2023; 10: 1096501.
[Crossref] [Google Scholar] [PubMed]
- Dagne AH, Zewude SB. Postpartum haemorrhage and associated factors among mothers who gave birth in South Gondar zone public health facilities, Ethiopia: A cross-sectional study. Postgrad Med J 2022; 98: 598-603.
[Crossref] [Google Scholar] [PubMed]
- Tolossa T, Fetensa G, Zewde EA, et al. Magnitude of postpartum hemorrhage and associated factors among women who gave birth in Ethiopia: A systematic review and meta-analysis. Reprod Health 2022; 19: 194.
[Crossref] [Google Scholar] [PubMed]
- Nigussie J, Girma B, Molla A, et al. Magnitude of postpartum hemorrhage and its associated factors in Ethiopia: A systematic review and meta-analysis. Reprod Health 2022; 19: 63.
[Crossref] [Google Scholar] [PubMed]