Current Pediatric Research
International Journal of Pediatrics
Pituitary stalk transection syndrome.
Gayathri S*
Department of Paediatrics, National Institute of Technology, Tiruchirappalli, India
- Corresponding Author:
- Gayathri S
Department of Paediatrics,
National Institute of Technology,
Tiruchirappalli,
India
E-mail: sgayathrisajeevan@gmail.com
Received: 11 September, 2020, Manuscript No. AAJCP-24-19055; Editor assigned: 16 September, 2020, Pre QC No. AAJCP-24-19055 (PQ); Reviewed: 30 September, 2020, QC No. AAJCP-24-19055; Revised: 01 November, 2024, Manuscript No. AAJCP-24-19055 (R); Published: 29 November, 2024, DOI: 10.35841/0971-9032.28.11.2394-2396.
Growth hormone deficiency is one of the most common endocrinological cause for short stature. It can either be idiopathic or associated with organic causes like tumors or following surgery. One of the rare cause for growth hormone deficiency in children is Pituitary Stalk Transection Syndrome (PSTS). It can be diagnosed by Magnetic Resonance Imaging (MRI) of the hypothalamus and pituitary gland which shows an ectopic or absent posterior pituitary, an absent or interrupted pituitary stalk or small anterior pituitary in combination with growth hormone or other pituitary hormone deficiencies. We present here a child with pituitary stalk transection syndrome who was brought for evaluation of hypoglycemic seizures.
Keywords
Growth hormone defeciency, Pituitary stalk transection syndrome, Short stature.
Introduction
Pituitary Stalk Transection Syndrome (PSTS) or pituitary stalk interruption syndrome is a rare congenital anomaly causing anterior pituitary deficiency with an incidence of 0.5/1,000,000 births. This was first described by Fujisawa et al in 1987. The classic triad of PSTS on MRI are thin or interrupted pituitary stalk, aplasia or hypoplasia of the anterior pituitary and absent or Ectopic Posterior Pituitary (EPP). The posterior pituitary function is usually normal. PSTS presents as isolated Growth Hormone Deficiency (GHD) or as Multiple anterior Pituitary Hormone Deficiencies (MPHD). It can be progressive with onset in childhood as a single hormone deficiency finally leading to pan-hypopituitarism later. Early diagnosis and management of the pituitary hormone deficiencies can decrease the mortality and morbidity. The data on this syndrome are mostly from western countries and no significant data is available from Asian countries. Here, we present a 5 year old male child who was brought for evaluation of hypoglycemic seizures in whom on detailed evaluation showed PSTS.
Case Presentation
5 year 3 month old developmentally normal male child born as 2nd child of NCM was brought for evaluation of 3 episodes of hypoglycemic seizures noted during early morning hours over the past two months. He had an uneventful antenatal period and was born by LSCS. Baby cried soon after birth. Birth weight was 4.3 kg. He had attained age appropriate milestones and had average scholastic performance. Many members of mothers family were short and they were intellectually normal.
On examination there were no obvious dysmorphic features or midline defects. Testes was bilaterally descended. His weight was 13.4 kg (at 3rd centile) and height was 95 cm (below 3rd centile). US:LS ratio was 1.12:1. Occipito frontal circumferance was normal. Mother’s height was 147 cm and father’s height was 170 cm. Mid parental height was 165 cm (between 10th and 25th centile). Stretch penile length was 3 cm. Tanner score was prepubertal and fundus examination was normal. There was no organomegaly.
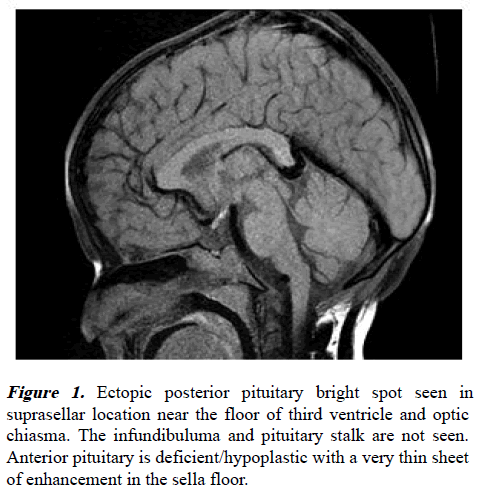
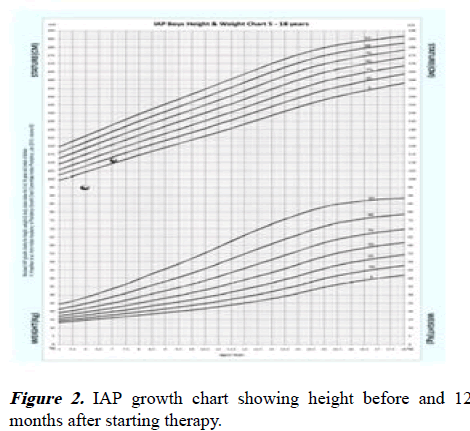
His investigations including complete hemogram, liver function tests, renal function tests, serum electrolytes and urine routine examination were normal. TFT was normal (Free T4-1.16 ng/dl, TSH-2.63 uIU/ml). Ultrasound abdomen was normal. Bone age corresponded to 2 years (against chronological age of 5 years 11 months and height age of 3 years). During the peak of hypoglycemic episode (RBS-37.8 mg/dl) which was induced for evaluation, critical samples were collected. His urine and blood ketones were positive. Serum insulin levels were <0.200 uIU/ml (3-35 uIU/ml), C-peptide levels-0.037 ng/ml (1.1-4 ng/ml), human growth hormone levels were low (0.198 ng/ml) and serum cortisol levels were normal (20.87 mcg/dl). Clonidine induced GH analysis was done. Growth hormone levels were found to be significantly low after stimulation (at 0 hours, 1 hours and 2 hours: 0.420 ng/ml, 0.491 ng/ml, 0.425 ng/ml). IGF-BP3 levels were reduced (IGF-BP3:934.25 ng/ml, normal value-1190-4200 ng/ ml). MRI brain pituitary protocol done showed ectopic posterior pituitary bright spot seen in suprasellar location near the floor of third ventricle and optic chiasma. The infundibulum and pituitary stalk are not seen. Anterior pituitary is deficient or hypoplastic with a very thin sheet of enhancement in the sella floor suggestive of PSTS. Thus the diagnosis of isolated growth hormone deficiency secondary to pituitary stalk transection syndrome was made. He was started on 0.24 mg/kg daily dose of inj. Norditropin. He was advised regular follow up for montoring growth and for other hormonal deficiencies (Figures 1 and 2).
Results and Discussion
PSTS usually presents during the first decade of life with a male to female sex ratio between 2.3 and 6.9:1. It can present as isolated growth hormone defeciency or associated with other multiple pituitary hormone deficiencies with onset in childhood [7].
The cause of PSTS is still unknown. PSTS can be due to defective migration of the pituitary gland during intrauterine life or trauma-related ischemia with subsequent reorganization of infundibular axons and development of an ectopic posterior pituitary. Many theories have been proposed like perinatal injuries, genetic or evironmental factors. Breech delivery causing deformation of head, hypoxia or anoxia after birth can also lead to injury of the pituitary stalk and pituitary. Midline malformations like cleft lip, absence of diaphragm, hypoplasia of optic nerve are seen in 20%-50% of the cases. Isolated GHD have a higher risk of congenital malformations as compared to those having multiple anterior pituitary deficiencies. Rarely mutations of HESX1, LH4, OTX3 and SOX3 are also seen. Current studies suggest that PSTS occurs as a direct or indirect consequence of the hypothalamic-pituitary lesion. Our patient had an uneventful natal, postnatal period and there were no associated malformations.
Clinical presentation varies depending on the age of diagnosis. In neonates it presents as neonatal hypoglycemia, prolonged neonatal (physiological) jaundice, cryptorchidism or micropenis. In older children and adults it is characterized by growth retardation and signs of anterior pituitory defeciency. Our patient presented with hypoglycemic seizures and had short stature on examination.
MRI findings of PSIS include hypoplasia or aplasia of anterior pituitary, absence of the hyper intense posterior lobe within the sella turcica and its presence at the level of the median eminence or at the pituitary stalk level as a hyper intense nodule and absent or thinned out pituitary stalk. There can be other variations in the MRI like the height of the anterior pituitary (from absence to normal), the appearance of the posterior pituitary lobe (ectopic at the base of the hypothalamus or along the pituitary stalk, absent or normal) and the form of the pituitary stalk (interrupted, thin, absent or normal) or even limited to an ectopic posterior pituitary. The position of the EPP is very significant. Anteriror pituitary hormone defeciencies are markedly increased when the posterior pituitory is present at the median eminence or at the hypothalamic region. In our patient, MRI pituitary protocol done showed ectopic posterior pituitary bright spot seen in suprasellar location near the floor of third ventricle and optic chiasma. The infundibulum and pituitary stalk are not seen. Anterior pituitary is deficient or hypoplastic with a very thin sheet of enhancement in the sella floor. On the basis of these findings, the diagnosis of PSTS was made. He was started on growth hormone therapy and is on regular follow up.
Conclusion
A high degree of suspicion is required for early diagnosis of growth hormone deficiency due to pituitary stalk transection syndrome. Early identification, initiation of therapy and strict growth monitoring is of paramount importance. Regular monitoring for multiple pituitary hormone deficiency should be looked out for. Close follow-up during pubertal period is necessary.
Author’s Contribution
GS reviewed the literature and drafted the initial manuscript. SN was involved in the management of the patient, designing the article, revision of manuscript and will act as a guarantor for the paper. NB, DG, CJK and SS were involved in the management of the patient and in critical revision of the manuscript.
Funding
None.
Competing Interest
None.
References
- El Chehadeh-Djebbar S, Callier P, Masurel-Paulet A, et al. 17q21. 31 microdeletion in a patient with pituitary stalk interruption syndrome. Eur J Med Genet 2011; 54: 369-373.
[Crossref] [Google Scholar] [PubMed]
- Fujisawa I, Kikuchi K, Nishimura K, et al. Transection of the pituitary stalk: Development of an ectopic posterior lobe assessed with MR imaging. Radiology 1987; 165: 487-489.
[Crossref] [Google Scholar] [PubMed]
- Simmons GE, Suchnicki JE, Rak KM, et al. MR imaging of the pituitary stalk: Size, shape and enhancement pattern. AJR Am J Roentgenol. 1992; 159: 375-377.
[Crossref] [Google Scholar] [PubMed]
- Tauber M, Chevrel J, Diene G, et al. Long-term evolution of endocrine disorders and effect of GH therapy in 35 patients with pituitary stalk interruption syndrome. Horm Res 2005; 64: 266-273.
[Crossref] [Google Scholar] [PubMed]
- Guo Q, Yang Y, Mu Y, et al. Pituitary stalk interruption syndrome in Chinese people: Clinical characteristic analysis of 55 cases. PloS One 2013; 8: e53579.
[Crossref] [Google Scholar] [PubMed]
- Pinto G, Netchine I, Sobrier ML, et al. Pituitary stalk interruption syndrome: A clinical-biological-genetic assessment of its pathogenesisd. J Clin Endocrinol Metab 1997; 82: 3450-3454.
[Crossref] [Google Scholar] [PubMed]
- Patkar D, Patankar T, Krishnan A, et al. MR imaging in children with ectopic pituitary gland and anterior hypopituitarism. J Postgrad Med 1999; 45: 81-83.
[Google Scholar] [PubMed]
- Melo ME, Marui S, Carvalho LR, et al. Hormonal, pituitary magnetic resonance, LHX4 and HESX1 evaluation in patients with hypopituitarism and ectopic posterior pituitary lobe. Clin Endocrinol 2007; 66: 95-102.
[Crossref] [Google Scholar] [PubMed]
- Simon D, Hadjiathanasiou C, Garel C, et al. Phenotypic variability in children with growth hormone deficiency associated with posterior pituitary ectopia. Clin Endocrinol 2006; 64: 416-422.
[Crossref] [Google Scholar] [PubMed]
- Wang CZ, Guo LL, Han BY, et al. Pituitary stalk interruption syndrome: From clinical findings to pathogenesis. J Neuroendocrinol 2017; 29.
[Crossref] [Google Scholar] [PubMed]