Current Pediatric Research
International Journal of Pediatrics
Meta-analysis and systematic review of under-five pneumonia in Ethiopia
Bizualem Abebaw, Destaw Damtie*
Department of Biology, Bahir Dar University, Bahir Dar, Ethiopia
- Corresponding Author:
- Destaw Damtie Department of Biology Bahir Dar University Bahir Dar Ethiopia E-mail: zegades96@gmail.com
Received: 30-Jun-2022, Manuscript No. AAJCP-22-68110; Editor assigned: 04-Jul-2022, AAJCP-22-68110 (PQ); Reviewed: 18-Jul-2022, QC No. AAJCP-22-68110; Revised: 30-Nov-2022, Manuscript No. AAJCP-22-68110 (R); Published: 28-Dec-2022, DOI: 10.35841/0971-9032.26.12.1744-1751
Background: In developing countries like Ethiopia, pneumonia is the leading cause of morbidity and mortality of under-five children. Ethiopia accounts for more than 18% of under-five deaths each year. However, there is a lack of evidence on the prevalence and risk factors of pneumonia among the under-five. This systematic review and meta-analysis aimed to determine the pooled prevalence of pneumonia and its associated risk factor among under-five children in Ethiopia.
Methods: We used articles published in Pubmed/Medline, science direct, web of science Google scholar, Hinari and Cochrane library. The authors incorporated observational studies (cross-sectional, retrospective and prospective) revealing the prevalence and factors associated with under-five pneumonia. We used STATA software version 14 for meta-analysis. We used the Cochrane Q test statistics and the I2 test to analyze the heterogeneity of the study. The study used the random-effect model to determine the pooled prevalence of pneumonia and associated factors among under-five children in Ethiopia.
Results: The pooled magnitude of pneumonia among under-five children was 18.03% (95% CI: 14.63, 21.44) out of 21 studies in Ethiopia. Cooking food in the living room (OR: 5.91, 95% CI: -0.36, 12.18), carrying children on mothers’ back during cooking (OR: 4.22%; 95%CI: 1.98, 6.45), child history of Acute Respiratory Infection (ARI) (OR: 3.51, 95% CI: 1.58, 5.44), children living in the overcrowded family (>5) members (OR: 3.48% CI: 0.87, 6.09), use of wood as a fuel source (OR: 2.58%; CI: 0.92, 4.23), being unvaccinated (OR: 2.52, 95% CI: 0.92, 4.23), non-exclusive breastfeeding (OR: 2.23; 95% CI: 0.87, 3.59) using charcoal and dung as fuel sources (OR: 1.89%; 95%CI: -0.51, 4.28) and kitchen without window (OR: 1.68% CI: -1.19, 4.54) were the risk factors associated with under-five pneumonia.
Conclusion: There existed a relatively high incidence of pneumonia in Ethiopia. We recommend public awareness about the effects of cooking places, keeping children during cooking, ARI management, family size, fuel type, breastfeeding and windows in the kitchen on children’s health.
Keywords
Under-five children, Pneumonia, Prevalence.
Introduction
Pneumonia is one form of Acute Lower Respiratory Infection (ALRI) that affects the lungs. Globally, it is the single most deadly infection of children. It has various causative agents. But severe cases are caused by bacteria (Streptococcus pneumoniae and Haemophilus influenza) [1].
The World Health Organization (WHO) defines pneumonia as a form of acute respiratory infection that affects the lungs [2]. Community Acquired Pneumonia (CAP) is an infection that begins outside the hospital or is diagnosed within 48 hours after admission to the hospital [3]. Hospital acquired pneumonia is pneumonia contracted by a patient in a hospital 48 hours after being admitted [4].
Globally, pneumonia is the leading cause of death among under-five children. In 2018 alone, it resulted in 802,000 underfive mortalities. This accounted to 162,000 under-five mortalities in Nigeria, 127,000 in India, 58,000 in Pakistan, 40,000 in democratic republic of the Congo, 32,000 in Ethiopia, 19,000 in Indonesia, 18,000 in China, 18,000 in Chad, 16,000 in Angola, 15,000 in United Republic of Tanzania, 15,000 in Somalia, 13,000 in Niger, 13,000 in Mali, 12,000 in Bangladesh and 11,000 in Sudan. Around 153,000 (19%) of the children died within their first month of age. It is close to 2,200 under-five mortalities per day and one child death every 39 seconds [5].
The annual global case of pneumonia reaches 1,400 cases per 100,000 children (one case per seventy-one children) [6]. From these cases, the highest incidence occurred in South Asia (2,500 cases per 100,000 children) and West and Central Africa (1,620 cases per 100,000 children) [7]. Sub-Saharan Africa had the highest under-five mortality rate, having an average underfive mortality rate of 172 deaths per 1,000 live births [8]. Out of fifteen countries with the highest death rates from clinical pneumonia in under-five children, Ethiopia ranks fourth in the world (84.6 deaths per 10,000 under-five population) [9].
In Ethiopia, the infant and under-five mortalities are 59 and 88 per 1000 live births, respectively. Of these, pneumonia causes 21% of the deaths [10]. Pneumonia contributes to 3,370,000 and 18% of the annual under-five morbidity and mortality, respectively [5].
The risk factors for pneumonia among under-five children in developing countries like Ethiopia are; socio-demographic status, malnutrition, non-exclusive breastfeeding during the first six months of age, lack of immunization, housing condition, tobacco smoking exposure, absence of a separate kitchen, kitchen without windows and environmental factors such as indoor air pollution, overcrowding, humidity, high altitude, co-morbid diseases and deficiencies of micronutrients like zinc, vitamin D and vitamin A [11-17].
Data on the prevalence of pneumonia and its risk factors are essential for planning child healthcare services. But such data are scarce in Ethiopia. It is also true about the prevalence and associated risk factors of pneumonia among under-five children. Thus, assessing the pooled prevalence of pneumonia and its risk factor at a country level is essential and will provide an overall figure with better estimation. Therefore, the main objective of this systematic review and meta-analysis is to estimate the pooled prevalence of pneumonia and its associated factor among under-five children in Ethiopia.
Literature Review
Methods
Study design and setting: A systematic review and metaanalysis study was employed to determine the prevalence and associated risk factors under-five pneumonia in Ethiopia.
Ethiopia, a country located in the horn of Africa, is bounded by Eritrea (North), Djibouti and Somalia (East), Sudan and South Sudan (West) and Kenya (South). The Ethiopian population (117,549,324) is equivalent to 1.47% of the global population.
Close to 21.3% (24,463,423 people in 2020) of the population is from urban areas. The median national age is 19.5 years. The population density in Ethiopia is 115 per Km2 (298 people per mi2) [18].
Search strategies: The authors searched articles written in English from online public databases (PubMed/MEDLINE, science direct, Google scholar, Hinari and world cat) [19,20].
They used core search terms and phrases: “prevalence,” “pneumonia,” “associated factors,” “under-five” and “Ethiopia.” These phrases were used either separately or in combination using “OR” or “AND.” Moreover, we searched for Gray literature through the review of available references.
The literature search took place from November 2020 to January 2021.
Inclusion and exclusion criteria: The present study included studies written in the English language, reporting about the prevalence of pneumonia and their associated risk factors among under-five children in Ethiopia, published from 2001 to January 2021, with sample sizes above 100 [20] and excluded studies conducted on HIV/AIDS patients and metaanalysis and review articles.
Data extraction: The authors prepared and evaluated the data extraction protocol. The data extraction protocol consists of the names of the authors and year of publication, region, nature of study subjects (patients, rural dwellers, kindergartens and urban dwellers), total sample size, number of positive cases, estimated prevalence and potential risk factors associated with under-five pneumonia.
Assessment of data quality: Grading of the Recommendations Assessment Development and Evaluation (GRADE) was employed to assess the overall data quality.
Each criterion was given two points. The qualities of the publications were rated as high (total score=4 points), moderate (total score=5-6 points) and low (total score=0-3 points) [20]. We used the log odds ratio to calculate the association between pneumonia and its associated risk factors.
We calculated the odds ratio for the common associated risk factors of the reported studies.
Outcomes of the study: The two outcome variables were the prevalence of under-five pneumonia and its associated factors.
Data analysis: A random effect model was applied to estimate the pooled prevalence of under-five pneumonia. After extraction of the articles in microsoft excel spread sheet format, we carried out the analysis using STATA version 14 statistical software. We assessed the heterogeneity among studies using Cochrane Q-test and I2 statistics [19]. This study employed sub-group analysis based on region, the study nature, year of publication and sample size; the forest plot format to present the pooled point prevalence with a 95% CI; and a log odds ratio to decide the association between associated factors and pneumonia among under-five children in the included studies [21].
Results
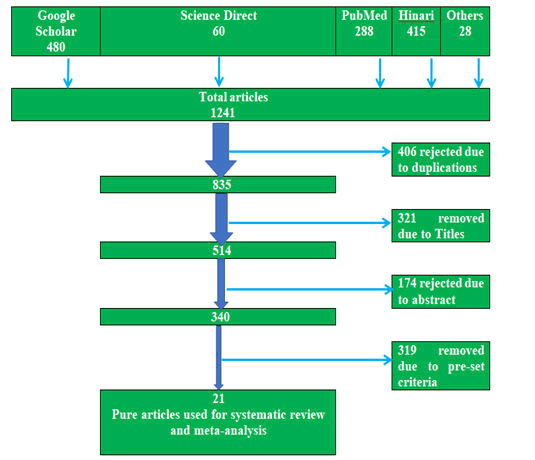
The authors retrieved a total of 1241 articles published from 2001 to January 2021 on the prevalence and associated risk factors of pneumonia among under-five children in Ethiopia from PubMed, Google scholar, science direct and Hinari search engines. From those articles, we excluded 406 due to duplications, 321 due to irrelevant titles, 174 due to irrelevant abstracts, 269 due to (lack of the prevalence of pneumonia, statistical outputs like odds ratio and 95% CI) and 319 due to pre-set criteria. Finally, we filtered 21 studies (n=14,525) for this systematic review and meta-analysis (Figure 1).
Characteristics of studies: The 21 selected studies included 14,525 study participants. We used this number of participants to determine the pooled prevalence of under-five pneumonia and its associated risk factors in Ethiopia. The sample size of the studies ranged from 206 to 5830 (Table 1) [11].
Eight (38.1%) of the studies were from the Amhara region, five (23.8%) from Southern Nations Nationalities and Peoples Region (SNNP), four (19.05%) from the Oromia region, 3(14.3%) from Addis Ababa and one (4.75%) from Harari.
However, we got no reports from Afar, Tigray, Dire-Dawa, Gambela, Somali and Benishangul Gumuz regions. Eighteen (85.7%) of the studies were cross-sectional, 2 (9.5%) retrospective and 1 (4.8%) prospective (Table 1).
The prevalence of under-five pneumonia ranged from 5.5% in the Debre Birhan district [12] to 39.6% in the Debre Birhan referral hospital, Amhara region. The quality score of each original study ranged from three to six (Table 1).
| No | Authors | Region | Study area | Study design | Sample size | case | Prevalence | Quality score |
|---|---|---|---|---|---|---|---|---|
| 1 | Fekadu et al. | Amhara | Estie town surrounding rural kebele | Cross-sectional | 286 | 46 | 16.10% | 6 |
| 2 | Alemayehu et al. | Amhara | Gondar city | Cross-sectional | 715 | 188 | 26.30% | 4 |
| 3 | Teka et al. | SNNPR | Bushulo major health center, Hawassa | Retrospective | 431 | 81 | 18.79 | 3 |
| 4 | Sanbata et al. | AA | Slum of Addis Ababa | Cross-sectional | 422 | 101 | 23.90% | 3 |
| 5 | Shibre | Amhara | Debre Birhan district | Cross-sectional | 458 | 25 | 5.50% | 6 |
| 6 | Desalegn | SNNPR | Shebedino Woreda | Cross-sectional | 405 | 85 | 21% | 3 |
| 7 | Abuka | SNNPR | Wondo genet district, Sidama zone | Cross-sectional | 206 | 69 | 33.50% | 6 |
| 8 | Tesfaye et al. | Oromia | Gumay district, Jimma | Cross-sectional | 347 | 26 | 7.50% | 5 |
| 9 | Wogderes et al. | AA | Yeka sub-city | Cross-sectional | 447 | 21 | 4.60% | 4 |
| 10 | Tegenu et al. | Oromia | Public hospitals in the Jimma zone | Cross-sectional | 306 | 86 | 28.10% | 6 |
| 11 | Tsegay and Biyadgie | SNNPR | Sheka zone | Cross-sectional | 560 | 133 | 23.80% | 4 |
| 12 | Negash et al. | AA | Tikur Anbessa and Yikatit 12 hospitals | Prospective observational | 549 | 31 | 5.65% | 4 |
| 13 | Abate | SNNPR | Tercha general hospital, Dawuro | Retrospective | 281 | 47 | 16.7 | 5 |
| 14 | Lema et al. | Oromia | Munesa district, Arsi zone | Cross-sectional | 344 | 61 | 17.70% | 6 |
| 15 | Abaye et al. | Oromia | district of Arsi Zone | Cross-sectional | 477 | 88 | 18.4 | 4 |
| 16 | Gizachew | Amhara | Debre Birhan Referral Hospital | Cross-sectional | 341 | 135 | 39.60% | 4 |
| 17 | Andualem et al. | Amhara | Gondar city | Cross-sectional | 792 | 95 | 12% | 6 |
| 18 | Adane et al. | Amhara | Biomass fuel using households | Cross-sectional | 5830 | 1120 | 19.21% | 3 |
| 19 | Bayu et al. | Harari | Hiwot Fana Specialized University Hospital | Cross-sectional | 384 | 43 | 11.20% | 3 |
| 20 | Gedif | Amhara | Dangila primary hospital | Cross-sectional | 384 | 68 | 17.7 | 3 |
| 21 | Keleb et al. | Amhara | Peri-urban area of Dessie city | Cross-sectional | 560 | 96 | 17.1 | 5 |
AA: Addis Ababa; SNNPR: Southern Nations Nationalities and People Region.
Table 1. Studies conducted in different parts of Ethiopia, their sample size and prevalence.
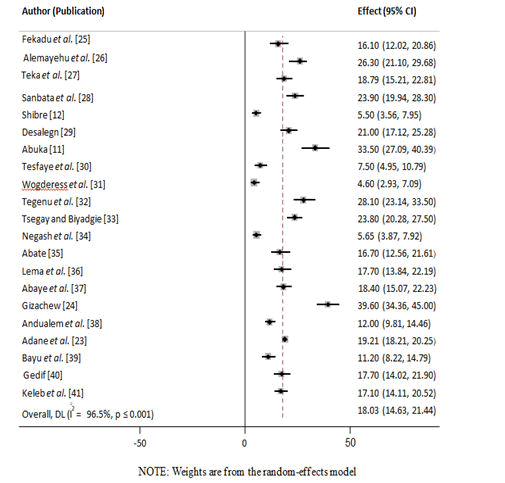
Prevalence of under-five pneumonia in Ethiopia: Based on the information from the 21 articles, the overall national prevalence of under-five pneumonia was 18.03% (95% CI: 14.63, 21.44) with a high heterogeneity across the included studies (I2=96.5%, P<0.001) (Figure 2).
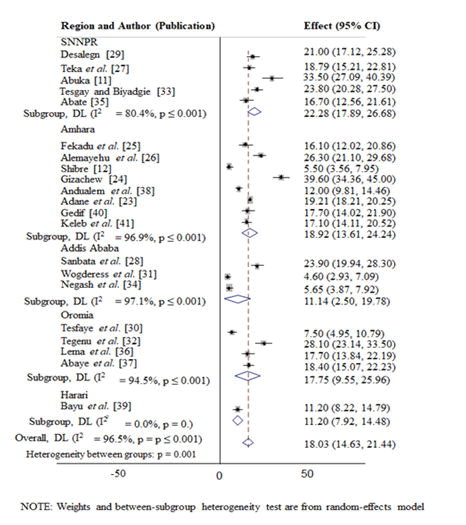
Sub-group prevalence of under-five pneumonia in Ethiopia: In the subgroup analysis, the highest prevalence of under-five pneumonia was observed in Sothern Nations Nationalities and Peoples Region (SNNPR) (22.28%; 95% CI=17.89, 26.68) followed by Amhara region (18.92%; 95% CI=13.61, 24.24), Oromia region (17.75%; 95% CI=9.55, 25.96), Harari (11.20%; 95% CI=7.92, 14.48) and addis ababa (11.14%; 95% CI=2.50, 19.78) in descending order (Figure 3 and Table 2).
| Variables | Characteristics | Included studies | Sample size | Prevalence with 95%CI | I2 |
|---|---|---|---|---|---|
| Region | Amhara | 8 (38.1%) | 9366 | 18.92% (13.61, 24.24) | 96.9%, p ≤ 0.001 |
| Oromia | 4 (19.05%) | 1474 | 17.75% (9.55, 25.96) | 94.5%, p ≤ 0.001 | |
| SNNPR | 5 (23.8%) | 1883 | 22.28% (17.89, 26.68) | 80.4%, p ≤ 0.001 | |
| Addis Ababa | 3 (14.3%) | 1418 | 11.14% (2.50, 19.78) | 97.1%, p ≤ 0.001 | |
| Harari | 1 (4.75%) | 384 | 11.20% (7.92, 14.48) | 0% | |
| Sample | ≤ 300 | 3 (14.3%) | 773 | 21.77% (12.29, 31.25) | 96.9%, p ≤ 0.001 |
| >300 | 18 (85.7%) | 13752 | 17.45% (13.77, 21.13) | 90.4%, p ≤ 0.001 | |
| Study year | 2001-2007 | - | - | - | |
| 2008-2014 | 4 (19.05%) | 1854 | 21.27% (16.82, 25.71) | 78.1%, p=0.003 | |
| 2015-2021 | 17 (80.95%) | 12671 | 17.29% (14.63, 21.44) | 97% p ≤ 0.001 | |
| Study nature | Patients | 8 (38.1%) | 2882 | 21.18% (13.42, 28.95) | 96.9%, p ≤ 0.001 |
| Urban dweller | 5 (23.8%) | 2936 | 16.62% (9.02, 24.23) | 97%, p ≤ 0.001 | |
| Rural dweller | 4 (19.05%) | 6926 | 16.31% (10.31, 22.31) | 94.8%, p ≤ 0.001 | |
| Urban and rural dweller | 3 (14.3%) | 1304 | 15.07% (3.13, 27.00) | 97.4%, p ≤ 0.001 | |
| Kindergarten students | 1 (4.75%) | 477 | 18.4% (14.82, 21.98) | 0% | |
| Study design | Cross-sectional | 18 (85.7%) | 13264 | 18.78% (15.11, 22.45) | 96.5%, p ≤ 0.001 |
| Retrospective | 2 (9.5%) | 712 | 17.93% (15.02, 20.84) | 0%, p=0.488 | |
| Prospective | 1 (4.75) | 549 | 5.65% (3.62, 7.68) | 0% | |
| Overall | 21 | 14525 | 18.03% (14.63, 21.44) | 96.5%, p ≤ 0.001 |
Table 2. Subgroup pooled prevalence of under-five pneumonia in Ethiopia.
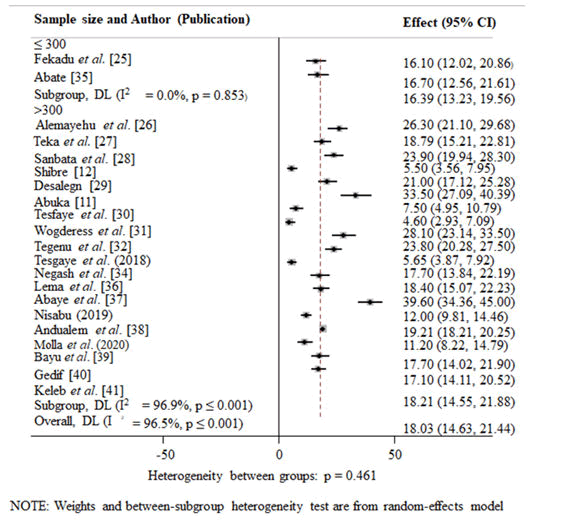
Effect of sample size on the prevalence of under-five pneumonia: Studies with a sample size of n ≤ 300 (21.77%; 95% CI=12.29, 31.25) had higher prevalence of under-five pneumonia than studies with sample sizes of n >300 (17.45%; 95%, CI=13.77, 21.13) (Figure 4).
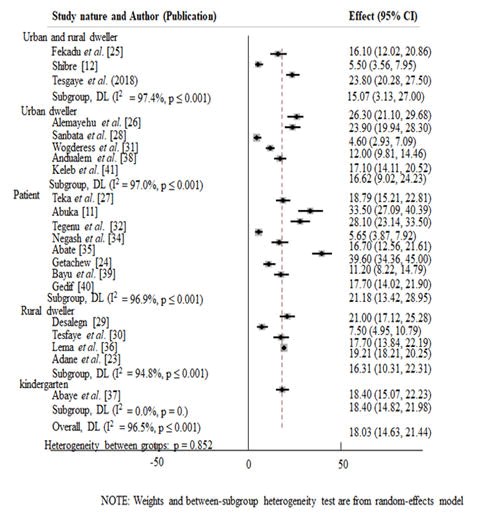
Prevalence of under-five pneumonia among the different groups of the study subjects: Under-five pneumonia prevalence varied among the different groups of the study subjects. It was highest among patients (21.18%) (95% CI=13.42, 28.95), followed by kindergarten attendants (18.4%) (95% CI=14.82, 21.98), urban dwellers (16.62%) (95% CI=9.02, 24.23), rural dwellers (16.31%) (95% CI=10.31, 22.31) and urban and rural dwellers (15.07%) (95% CI=3.13, 27.00) in descending order (Figure 5).
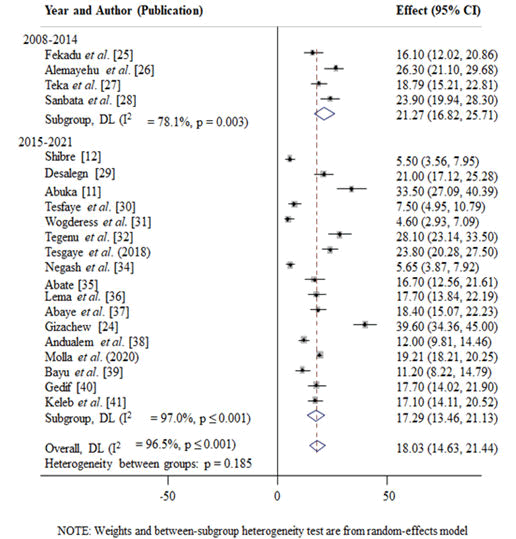
Temporal difference of the prevalence of under-five pneumonia in Ethiopia: Additionally, the prevalence of under-five pneumonia from years 2001 to 2007 was 0%, from 2008 to 2014 (21.27%; 95% CI=16.82, 25.71) and from years 2015 to 2021 (17.29%; 95% CI=14.63, 21.44) (Figure 6).
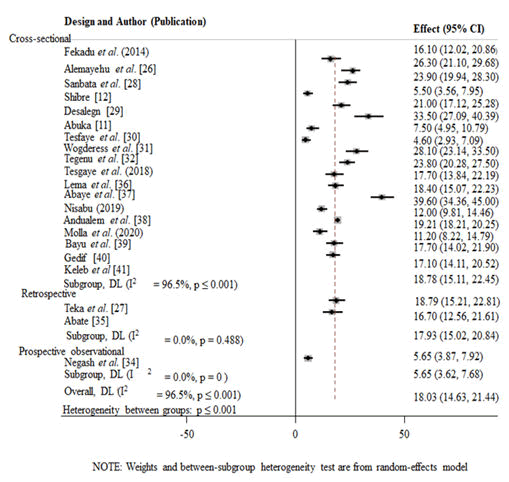
The study design-dependent variation of the prevalence of under-five pneumonia in Ethiopia: The prevalence of underfive pneumonia was (18.78%) (95% CI=15.11, 22.45) among cross-sectional studies, (17.93%) (95% CI=15.02, 20.84) among retrospective studies and (5.65%) (95% CI=3.62, 7.68) in prospective studies in descending order (Figure 7).
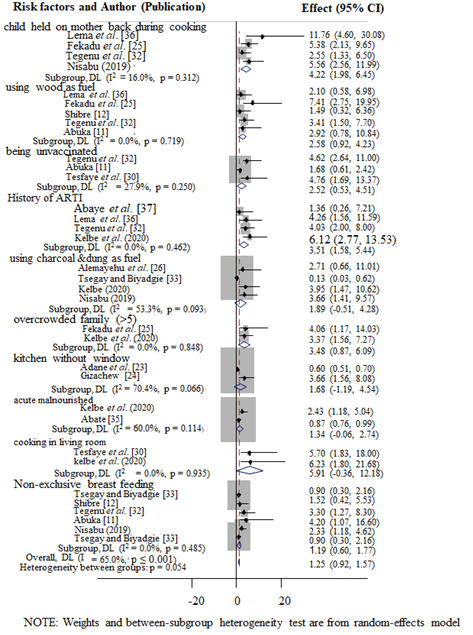
Factors associated with pneumonia among different groups of under-five children in Ethiopia: Four studies stated the prevalence of pneumonia among under-five children usually held at their mothers’ backs during cooking. The odds of under-five pneumonia were 4.22 times higher among children who used to be held at their mothers’ backs during cooking when compared to their counterparts (OR: 4.22%; 95%, CI: 1.98, 6.45; I2=16%; P=0.312) (Figure 8).
Six studies evaluated the association between breastfeeding and under-five pneumonia. The odds of having pneumonia were 2.23 times higher among children who were nonexclusive breast-feeders than exclusive breast-feeders (OR: 2.23; 95% CI: 0.87, 3.59; I2=47.5%; P=0.09) (Figure 8).
The authors analyzed the associations between using wood as a fuel source and under-five pneumonia using five studies. The odds of under-five pneumonia were 2.58 times higher among wood users than electric power users (OR: 2.58%; CI: 0.92, 4.23; I2=0%; P=0.719).
Meta-analysis of three studies revealed that under-five children who were unvaccinated were 2.52 times more likely to have pneumonia than those who were vaccinated (OR: 2.52, 95% CI: 0.92, 4.23; I2=27.9%, P=0.25).
In the meta-analysis of the four studies, an association was existed between having a history of ARI and under-five pneumonia. The overall meta-analysis report showed that having a history of ARI was 3.51 times more associated with pneumonia than those who hadn’t a history of ARI (OR: 3.51, 95% CI: 1.58, 5.44; I2=0%; P=0.462).
The following four studies reported the association between using charcoal and dung as a source of fuel and under-five pneumonia. Using charcoal and dung as a source of fuel increases pneumonia risk 1.89 times higher than using electric power (OR: 1.89%; 95%CI: -0.51, 4.28; I2=53.3%; P=0.093).
We used the studies conducted by Gizachew N and Adane MM, et al. to analyze the association between kitchens without windows and under-five pneumonia. The odds of kitchen without windows were 1.68 times higher occurrence of pneumonia than kitchen with windows (OR: 1.68% CI: -1.19, 4.54; P=0.066; I2=70.4%; P=0.066.
Meta-analysis of two studies showed that children living in the overcrowded family were 3.48 times at a higher risk of underfive pneumonia compared to those who live in less than five family size (OR: 3.48% CI: 0.87, 6.09; P=0.848).
Meta-analysis of two studies revealed that under-five children who were acute malnourished were 1.34 times more likely to have pneumonia than those who were well-nourished (OR: 1.34, 95% CI: -0.06, 2.74; I2=60%, P=0.114).
Finally, we computed the association between cooking in the living room and pneumonia among under-five children in Ethiopia using the reports of Tesfaye, et al. and Keleb, et al. The overall meta-analysis report showed that cooking in the main house was 5.91 times riskier than having separate kitchens (OR: 5.91, 95% CI: -0.36, 12.18; P=0.935).
Discussion
This meta-analysis resulted in an 18.03% pooled prevalence of pneumonia among under-five children in Ethiopia. The result is in line with the studies conducted in India (16.34%) and Somalia (17%), higher than studies from Vienna, Austria (4.1%), Mali (6.7%), Uganda (6.9%), Kenya (6.9%) and lower than the findings from Sudan (20.2%), Bangladesh (21.3%) and Nigeria (31.6%). These variations may be due to differences in socioeconomic or demographic status, season, immunization and vitamin A supplementation [14]. Thus, in low and middle-income countries, pneumonia remains the leading cause of childhood mortality and hospitalization.
Region wise, the highest prevalence of under-five pneumonia was observed in SNNPR (22.28%) (95% CI: 17.89, 26.68) and the lowest in Addis Ababa (11.14%) (95% CI: 2.50, 19.78). It may be due to differences in sanitary, health and energy facilities. Addis Ababa is the capital city of Ethiopia, containing much of the infrastructure. Patients (21.18%) (95% CI: 13.42, 28.95) and the urban and rural dwellers (15.07%) (95% CI: 3.13, 27.00) were the highest and the lowest affected groups, respectively. The reason may probably be because patients (children with weakened immune systems) are at greater risk of developing pneumonia [2].
The odds of pneumonia occurrence were 4.22 times higher among under-five children who used to be held on the back of their mothers during cooking when compared with their counterparts (OR: 4.22%; 95%, CI: 1.98, 6.45; P=0.312). It was in line with a survey conducted in Nepal. It may be because high indoor air pollution associated with fuel use adversely affects specific and non-specific host defences of the respiratory tract against pathogens. Improved household air quality can reduce cases of severe pneumonia.
The odds of pneumonia were 2.23 times higher among underfive children who were non-exclusive breast feeders than exclusive breast feeders (OR: 2.23; 95% CI: 0.87, 3.59). The study conducted in India supports the present finding. Pieces of evidence showed that Breastfed infants have a larger thymus at four months of age than those not breastfed, have higher titters of neutralizing antibodies post-vaccination and may mount more effective immune responses. Immunoglobulin antibodies from breast milk also protect against infection by neutralizing pathogens at mucosal surfaces.
The odds of pneumonia in under-five children whose family uses wood as fuel sources were 2.58 times higher than nonusers (OR: 2.58%; CI: 0.92, 4.23). This result was in line with studies conducted in India and Sri Lanka. The association between wood use as a source of fuel and pneumonia in underfive children might be because using wood as a source of fuel results in the release of wood smokes containing major air pollutants like carbon monoxide and particulate matter that causes indoor air pollution.
Children who had ARI in the last two weeks were 3.51 times more at risk to develop pneumonia than their counterparts (OR: 3.51, 95% CI: 1.58, 5.44). It was in line with that of Kenya. It probably might be due to respiratory tract infections being easily transmitted from household contacts to children. The severity of the disease also depends on the virulence and load of the pathogen. The pathogen load is usually higher when the infection is from a household contact.
Acute malnourished under-five children were 1.34 times more likely to develop pneumonia than well-nourished (OR: 1.34, 95% CI: -0.06, 2.74). It is in line with a study conducted in India which showed that pneumonia was significantly associated with malnutrition. It may be because malnutrition compromises the overall immune system of children.
Furthermore, under-nourished children have weakened respiratory muscles, preventing them from adequately clearing secretions found in their respiratory tracts.
Unvaccinated children were 2.52 times more likely to develop pneumonia when compared with fully vaccinated children (OR: 2.52, 95% CI: 0.92, 4.23). It is consistent with a study undertaken in two slums of Dibrugarh town, India. It is due to immunizations helping to reduce childhood pneumonia.
Finally, cooking foods in the living rooms resulted in higher odds of pneumonia than cooking food in the kitchen (OR: 5.91, 95% CI: -0.36, 12.18). It is in line with the study conducted in Seri Lank. The explanation for this association may be that cooking food in the living rooms induces indoor air pollution, which raises the risk of pneumonia by altering the structure and function of the respiratory tract.
Limitation
The authors failed to get published articles about the prevalence of under-five pneumonia from Gambela, Somali, Tigray, Afar, Dire Dewa and Benishangul Gumuz regions. So, the reported overall prevalence in Ethiopia is excluding the mentioned regions.
Conclusion
According to this systematic review and meta-analysis, the overall pooled prevalence of under-five pneumonia is 18.03%. The associated risk factors of under-five pneumonia in Ethiopia are; cooking food in the living room, carrying a child on the back of the mother during cooking, being unvaccinated, non-exclusive breastfeeding, child history of ARI, kitchen without window, use of wood as a fuel source and living in overcrowded families. To prevent the identified risk factors, we recommend appropriate interventions such as health education about exclusive breastfeeding and nutrition, place of food cooking, increased immunization and vitamin A supplementation and early control of acute respiratory infections.
References
- Abbott MB, Vlasses CH. Nelson textbook of pediatrics. JAMA. 2011;306(21):2387-88.
[Crossref]
- Shebl E, Gulick PG. Nosocomial Pneumonia. StatPearls. 2020.
- Black RE, Cousens S, Johnson HL, et al. Global, regional and national causes of child mortality in 2008: a systematic analysis. The lancet. 2010;375(9730):1969-87.
- Temesgen D, Bereded F, Derbie A, et al. Bacteriology of community acquired pneumonia in adult patients at Felege Hiwot Referral Hospital, Northwest Ethiopia: A cross-sectional study. Antimicrob Resist Infect Control. 2019;8(1):1-8.
- Roomaney RA, Pillay-van Wyk V, Awotiwon OF, et al. Epidemiology of lower respiratory infection and pneumonia in South Africa (1997–2015): A systematic review protocol. BMJ open. 2016;6(9):e012154.
- Alamneh YM, Adane F. Magnitude and Predictors of Pneumonia among Under-Five Children in Ethiopia: A Systematic Review and Meta-Analysis. J Environ Public Health. 2020;2020:1-9.
- Moher D, Pham B, Lawson ML, et al. The inclusion of reports of randomised trials published in languages other than English in systematic reviews. Health Technol Assess. 2003;7(41):1-90.
- Tegen D, Damtie D, Hailegebriel T, et al. Prevalence and Associated Risk Factors of Human Intestinal Protozoan Parasitic Infections in Ethiopia: A Systematic Review and Meta-Analysis. J Parasitol Res. 2020;2020:1-15.
- Alemnew B, Gedefaw G, Diress G, et al. Prevalence and factors associated with intestinal parasitic infections among food handlers working at higher public University student’s cafeterias and public food establishments in Ethiopia: A systematic review and meta-analysis. BMC Infect Dis. 2020;20(1):1-2.
- Atkins D, Eccles M, Flottorp S, et al. Systems for grading the quality of evidence and the strength of recommendations I: Critical appraisal of existing approaches The GRADE Working Group. BMC Health Serv Res. 2004;4(1):1-7.
- Rücker G, Schwarzer G, Carpenter JR, et al. Undue reliance on I2 in assessing heterogeneity may mislead. BMC Med Res Methodol. 2008;8(1):1-9.
- Adane MM, Alene GD, Mereta ST, et al. Prevalence and risk factors of acute lower respiratory infection among children living in biomass fuel using households: A community-based cross-sectional study in Northwest Ethiopia. BMC Public Health. 2020;20(1):1-3.
- Sanbata H, Asfaw A, Kumie A. Association of biomass fuel use with acute respiratory infections among under-five children in a slum urban of Addis Ababa, Ethiopia. BMC Public Health. 2014;14(1):1-8.
- Bayu D, Mekonnen A, Mohammed J, et al. Magnitude of Streptococcus pneumoniae Among Under-Five Children with Symptom of Acute Respiratory Infection at Hiwot Fana Specialized University Hospital, Harar, Ethiopia: Associated Risk Factors and Antibacterial Susceptibility Patterns. Risk Manag Healthc Policy. 2020;13:2919.
- Keleb A, Sisay T, Alemu K, et al. Pneumonia remains a leading public health problem among under-five children in peri-urban areas of north-eastern Ethiopia. PloS one. 2020;15(9):e0235818.
- Nirmolia N, Mahanta TG, Boruah M, et al. Prevalence and risk factors of pneumonia in under five children living in slums of Dibrugarh town. Clin Epidemiol Glob Health. 2018;6(1):1-4.
- Kinyoki DK, Manda SO, Moloney GM, et al. Modelling the ecological comorbidity of acute respiratory infection, diarrhoea and stunting among children under the age of 5 years in Somalia. Int Stat Rev. 2017;85(1):164-76.
- Kurz H, Göpfrich H, Huber K, et al. Spectrum of pathogens of in-patient children and youths with community acquired pneumonia: A 3 year survey of a community hospital in Vienna, Austria. Wien klin Wochenschr. 2013;125(21):674-9.
- Bénet T, Sylla M, Messaoudi M, et al. Etiology and factors associated with pneumonia in children under 5 years of age in Mali: A prospective case-control study. PloS One. 2015;10(12):e0145447.
- Tuhebwe D, Tumushabe E, Leontsini E, et al. Pneumonia among children under five in Uganda: Symptom recognition and actions taken by caretakers. Afr Health Sci. 2014;14(4):993-1000.
- Hammitt LL, Kazungu S, Morpeth SC, et al. A preliminary study of pneumonia etiology among hospitalized children in Kenya. Clin Infect Dis. 2012;54:S190-9.