Current Pediatric Research
International Journal of Pediatrics
Introduction: Acute Kidney Injury (AKI) is associated with severe morbidity and mortality. Lack of consensus definition has been major limitation in improving outcomes. Acute Dialysis Quality Initiative Group (ADQI) group proposed RIFLE (Risk, Injury, Failure, Loss of function, End stage renal disease) criteria, criteria for defining AKI, later modified in children as pRIFLE (pediatric RIFLE). This study tries to address the need of limited data on pediatric AKI.
Methodology: A prospective study conducted in between December 2013 to May 2015. Serum creatinine level was estimated on all patients on admission and alternate days till discharge from Pediatric Intensive Care Unit (PICU). Urine output was recorded. Estimated Creatinine- Clearance (eCrCL) was calculated using Schwartz formula. AKI diagnosis and staging was based on pRIFLE (pediatric RIFLE) criteria. Either eCrCl or urine output criteria were used to diagnose and stage AKI, using criterion that leads to higher stage. Maximal stage that the patient progressed during the stay in PICU was assigned the stage for that case. Data was compiled using SPSS software.
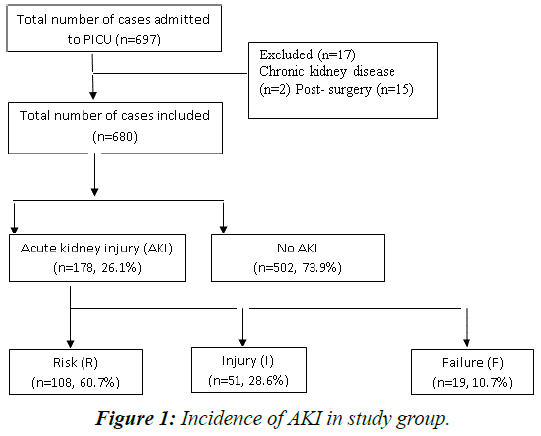
Results: Of total 697 cases, 680 cases met inclusion criteria. Incidence of AKI was 178 (26.1%). Stage ‘Risk (R)’, ‘Injury (I)’ and ‘Failure (F)’ constituted 60.7% (108), 28.6% (51) and 10.6% (19) respectively. Maximum AKI occurred in < 1 year (28.1%) (p=0.003). Urine output and creatinine criteria matching were there in 77%. Infections were commonest etiology. Amongst infections dengue (30%) was most common, followed by sepsis (21.9%) and then pneumonia (17.9%). Hypotension, nephrotoxic drugs, sepsis, need for mechanical ventilation were significant (p<0.001) risk factors for AKI. Prerenal causes constituted 68% and renal 32%.
Conclusion: Incidence of AKI is high among critically ill children. pRIFLE staging system that provides early identification and stratification of AKI. Infections are leading etiology of AKI in children.
Keywords
AKI, pRIFLE, PICU
Introduction
Acute Kidney Injury (AKI) has become a major global health care challenge with an estimated 13.3 million cases per year leading to an estimated mortality of 1.7 million deaths per year globally. Increasing prevalence of AKI is strongly associated with increased early and long term patient morbidity and mortality [1]. According to recent meta-analysis conducted by Paweena et al the pooled incidence rate of AKI was 33.7% (95% CI, 26.9 to 41.3) and AKI-associated mortality rates was 13.8% in children (95% CI, 8.8 to 21.0) [2].
“0 by25” is an ambitious initiative of International Society of Nephrology which aims to eliminate preventable deaths from Acute Kidney Injury worldwide by 2025. This initiative emphasizes the magnitude of the problem, the global concern about AKI and its endeavour to eliminate mortality and morbidity due to AKI.
Acute kidney injury previously called acute renal failure is characterized by a reversible increase in the blood concentration of creatinine and nitrogenous waste products and by the inability of the kidney to appropriately regulate fluid and electrolyte homeostasis [3]. If left untreated, the condition has a high risk of multiple organ failure and potentially death. Patients who suffer from AKI may have subsequent renal dysfunction after original injury. Children are more susceptible for this dysfunction [4].
For a long time there was lack of consensus on definition of AKI. In 2005, the first consensus definition of AKI for the adult population, based on the RIFLE (Risk, Injury, Failure, Loss of function, End stage renal disease) criteria, was proposed by the Acute Dialysis Quality Initiative Group (ADQI) [5]. The definition was later modified and evaluated in critically ill pediatric patients and termed pRIFLE (Pediatric RIFLE) criteria. The pRIFLE criteria differs from RIFLE criteria, in that a) Only decrease in estimated creatinine clearance (eCrCL), and not the change in glomerular filtration rate, is used to determine grading b) The eCrCl is estimated using the Schwartz formula, which incorporates the height and serum creatinine level of the patient, and an age adjusted constant c) pRIFLE incorporates a longer duration of urine output than in adult RIFLE classification.
The spectrum and burden of AKI in developing countries may be different from that of developed countries [6] The patients from developing countries are younger, infection associated AKI is more common and a significant proportion may have already developed AKI at the time of hospitalization. In addition, resource limitations in managing children who require renal replacement therapy add to the burden [7,8].
Most of the studies in AKI are based on adult population. The incidence and clinico-etiological profile of AKI varies from adults to children. Of the pediatric studies on incidence of AKI, many are limited to developed countries and often retrospective [9]. Hence limited data availability on clinical profile of pediatric AKI from Indian children, fallacies of retrospective studies, and regional variations in the profile of AKI makes it compelling to study incidence and outcome of AKI in pediatric patients and current study tries to address this need.
Methodology
This was a Prospective and observational study conducted at Kempegowda Institute of Medical Sciences, Bangalore. All patients within the age group of 1 month to 18 years admitted to Pediatric Intensive Care Unit (PICU) in between December 2013 to May 2015 were included in the study. Patients with known kidney disease and postoperative cases were excluded from the study.
The study was approved by the Institute Ethics Committee. Informed consent was taken from parents of all participants. Detailed clinical history and examination was done, co-morbidities were noted, and relevant data regarding investigations was collected for all children admitted to PICU.
Serum creatinine levels were estimated by modified Jaffe method, which is quick, simple, reliable and inexpensive method of creatinine estimation [10]. Serum creatinine was estimated on all patients admitted to PICU on the day of admission and on alternate days till discharge from PICU. Serum creatinine may be repeated frequently in children who develop shock, sepsis, need for ventilation, inotropes or diuretics. Creatinine estimation was done at daily intervals in those patients with AKI.
Estimated creatinine clearance (eCrCL) was calculated using Schwartz formula [11]. Age related creatinine clearance was taken as the baseline CrCl.
Urine output measured and recorded as ml/kg/hour. Only patients who were catheterized were considered for urine output criteria.
Diagnosis and staging of AKI was based on Pediatric RIFLE definition & classification. Either eCrCl or urine output was used to diagnose and stage AKI, using a criterion that leads to higher stage classification. Shock was defined in presence of tachycardia, feeble pulses, cool peripheries, hypotension (blood pressure <-2 Standard deviation (SD) for age and sex) or capillary filling time > 3 seconds. Sepsis was the presence of systemic inflammatory response syndrome with suspected or proven infection [11]. The diagnosis of prerenal vs renal was decided based on clinical diagnosis and supported by progressively increasing serum creatinine values, even after 48 hours of admission and appropriate fluid therapy (Table 1).
| Estimated Creatinine Clearance (eCrCl) | Urine output | |
|---|---|---|
| Risk | decrease by 25% | <0.5 ml/kg/h for 8 h |
| Injury | decrease by 50% | <0.5 ml/kg/h for 16 h |
| Failure | decrease by 75% or eCrCl<35 ml/min/1.73 m2 | <0.3 ml/kg/h for 24 h or anuric for 12 h |
| Loss | Persistent failure >4 weeks | |
| End stage | End-stage renal disease (persistent failure >3 months) |
Table 1: Classification/staging system for acute kidney injury.
Estimated GFR for children is calculated using SCHWARTZ formula
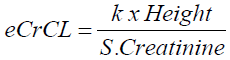
k = 0.45 for infants 1 to 52 weeks old
k = 0.55 for children 1 to 13 years old
k = 0.55 for adolescent females 13-18 years old
k = 0.7 for adolescent males 13-18 years old
The maximal stage that the patient progressed during the stay in PICU was assigned the final stage for that case. The patients were evaluated to ascertain the etiology of AKI and its progression and were followed until discharge.
Statistical analysis
The incidence of AKI in children is approximately 5% among non-critically ill and 30% in critically ill according to Basu and Askenazi et al [4,12].
In order to estimate these incidence rates at 95% confidence, and precision of 2.5% for the non-critically ill and 9% for critically ill, the minimum required sample sizes were 304 and 104, respectively (Formula used is n=z21-α/2 P(1-P)/€2 where z= 95% power and 5% level of significance (1.96), P is the incidence, €= Absolute precision).The admissions to our PICU in previous year were well above the minimum required sample. Hence all the cases in the study period were considered.
Descriptive and inferential statistical analysis has been carried out in the present study. Results on continuous measurements are presented on Mean ± SD (Min-Max) and results on categorical measurements are presented in Number (%). Significance is assessed at 5% level of significance. Student t test (two tailed, independent) has been used to find the significance of study parameters on continuous scale between two groups (Inter group analysis) on metric parameters. Chi-square/ Fisher Exact test has been used to find the significance of study parameters on categorical scale between two or more groups. Multivariate Logistic regression analysis was done to assess the risk factors for development of AKI.
Statistical software
The Statistical software namely SAS 9.2, SPSS 15.0, Stata 10.1, MedCalc 9.0.1, Systat 12.0 and R environment ver.2.11.1 were used for the analysis of the data and Microsoft word and Excel have been used to generate graphs, tables etc.
Results
A total of 697 cases were admitted during the study period. Of these 17 cases were excluded and 680 cases were included in the study.
In this study, out of 680 included patients admitted to PICU during the study period 178 had AKI making an incidence of 26.1%. Stage ‘Risk’ comprised maximum cases with 60.7% (108 cases), followed by ‘Injury’ comprised 28.6% (51 cases) and ‘Failure’ comprised 10.6% (19 cases). Maximum AKI occurred in <1 year (28.1%) and incidence was highest among younger age group (p=0.003) (Figure 1).
Amongst the AKI cases creatinine criteria was used in all cases while urine output criteria was applied for 190 cases. RISK (R), INJURY (I) and FAILURE (F) cases were 108 (60.7%), 51(28.6%) and 19(10.7%) respectively by eCrCL criteria. For urine output criteria, 74 cases of the 190 cases had AKI. Among these 74 cases incidence of stage ‘R’ was 31%. ‘I’ was 46% and ‘F’ was 23% respectively (Table 2).
| Stage | Creatinine Criteria | Urine output Criteria | ||||
|---|---|---|---|---|---|---|
| No AKI | AKI | Total | No AKI | AKI | Total | |
| No AKI | 502(100%) | 0(0%) | 502(73.8%) | 116(100%) | 0(0%) | 116(61.1%) |
| Risk | 0(0%) | 108(60.7%) | 108(15.9%) | 0(0%) | 23(31.1%) | 23(12.1%) |
| Injury | 0(0%) | 51(28.6%) | 51(7.5%) | 0(0%) | 34(45.9%) | 34(17.9%) |
| Failure | 0(0%) | 19(10.7%) | 19(2.8%) | 0(0%) | 17(23.0%) | 17(8.9%) |
| Total | 502(100%) | 178(100%) | 680(100%) | 116(100%) | 74(100%) | 190(100%) |
Table 2: Creatinine and urine output criteria stage in relation to incidence of AKI.
Urine output criteria was applied for 74 of all AKI cases and there was matching between urine output and creatinine criteria in 57 cases (77%). There was 39.1% matching in stage ‘RISK’, 91.2% in stage ‘INJURY’ and 100% in stage ‘FAILURE’ (Table 3).
| Final Rifle stage | Urine output stage (U) | Total | ||
|---|---|---|---|---|
| RU | IU | FU | ||
| Risk | 9(39.1%) | 1(2.9%) | 0(0%) | 10(13.5%) |
| Injury | 14(60.9%) | 31(91.2%) | 0(0%) | 45(60.8%) |
| Failure | 0(0%) | 2(5.9%) | 17(100%) | 19(25.7%) |
| Total | 23(100%) | 34(100%) | 17(100%) | 74(100%) |
Table 3: Matching between creatinine criteria staging and urine output staging.
In this study maximum AKI occurred in <1 year and incidence was highest among younger age group (p=0.003) (Table 4).
| Age in years | Final Rifle Stage | Total | |
|---|---|---|---|
| No AKI | AKI | ||
| <1 yr | 110(21.9%) | 50(28.1%) | 160(23.5%) |
| 1-2 yrs | 96(19.1%) | 35(19.7%) | 131(19.3%) |
| 2-5 yrs | 86(17.1%) | 43(24.2%) | 129(19%) |
| 5-10 yrs | 71(14.1%) | 27(15.2%) | 98(14.4%) |
| 10-15 yrs | 97(19.3%) | 18(10.1%) | 115(16.9%) |
| >15 yrs | 42(8.4%) | 5(2.8%) | 47(6.9%) |
| Total | 502(100%) | 178(100%) | 680(100%) |
Table 4: Association of Age in years in relation to incidence of AKI.
Infections were the leading cause of AKI. Amongst infections dengue (30%) was the most common etiology associated with AKI, followed by sepsis (21.9%) and then pneumonia (17.9%) (Table 5).
| AKI etiology | AKI cases | |
|---|---|---|
| Number | Percentage | |
| Dengue | 54 | 30.0 |
| Pneumonia | 32 | 17.9 |
| Sepsis | 39 | 21.9 |
| Acute GE | 9 | 5.05 |
| HUS | 4 | 2.24 |
| ALS | 10 | 5.61 |
| Poisoning | 15 | 8.42 |
| Status epilepticus | 7 | 3.9 |
| Malignancy | 2 | 1.12 |
| Snake bite | 2 | 1.12 |
| Cardiac Failure | 4 | 2.24 |
Table 5: Etiology of AKI.
On univariate analysis, hypotension, nephrotoxic drugs, sepsis, need for mechanical ventilation were significant risk factors for AKI. 56.9% of patients with AKI were boys. (p=0.818). There was no significant difference of AKI between males and females Hypotension was found in 75.3% of patients with AKI (p<0.001). Nephrotoxic drugs were associated with 42.1% of AKI cases (p<0.001). Sepsis was present in 21.9% of AKI cases (p<0.001). Need for mechanical ventilation was there in 20.2% cases (p<0.001) (Table 6).
| Variables | Final Rifle stage | Total (n=680) | P value | |
|---|---|---|---|---|
| No AKI (n=502) | AKI (n=178) | |||
| Gender | ||||
| • Male | 287(57.2%) | 100(56.2%) | 387(56.9%) | 0.818 |
| • Female | 215(42.8%) | 78(43.8%) | 293(43.1%) | |
| Hypotension | ||||
| • Yes | 154(30.7%) | 134(75.3%) | 288(42.4%) | <0.001 |
| • No | 348(69.3%) | 44(24.7%) | 392(57.6%) | |
| Nephrotoxic drugs | ||||
| • Yes | 291(58%) | 75(42.1%) | 366(53.8%) | <0.001 |
| • No | 211(42%) | 103(57.9%) | 314(46.2%) | |
| Sepsis | ||||
| • Yes | 52(10.4%) | 39(21.9%) | 91(13.4%) | <0.001 |
| • No | 450(89.6%) | 139(78.1%) | 589(86.6%) | |
| Ventilator | ||||
| • Yes | 34(6.8%) | 36(20.2%) | 70(10.3%) | <0.001 |
| • No | 468(93.2%) | 142(79.8%) | 610(89.7%) | |
Table 6: Correlation of clinical variables in relation to incidence of AKI.
In this study, of all the AKI cases 68% were due to Prerenal cause and 32% was renal cause (Table 7).
| Cause of AKI | No. of patients | % |
|---|---|---|
| Pre Renal | 121 | 68.0 |
| Renal | 57 | 32.0 |
| Total | 178 | 100.0 |
Table 7: Cause of AKI in relation to incidence of AKI in patients studied.
A Backward Wald logistic regression was performed to ascertain the effects of hypotension, Sepsis, Ventilation and nephrotoxic drugs usage on the likelihood that participants have acute kidney injury. The logistic regression model was statistically significant P<0.001 drawing an inference that each of these risk factors were individually associated with occurrence of AKI (Table 8).
| Variables | Logistic regression results to predict the development of AKI | 95%CI | |||||
|---|---|---|---|---|---|---|---|
| Logit co-efficient | SE | Wald | P value | Adj OR | Lower | Upper | |
| Hypotension | 1.78 | 0.21 | 70.95 | <0.001 | 5.95 | 3.93 | 9.01 |
| Nephrotoxic drugs | -0.79 | 0.20 | 15.28 | <0.001 | 0.45 | 0.31 | 0.67 |
| Sepsis | 0.91 | 0.27 | 11.81 | 0.001 | 2.50 | 1.48 | 4.20 |
| ventilation | 0.62 | 0.29 | 4.51 | 0.034 | 1.85 | 1.05 | 3.28 |
Table 8: Multivariate Logistic regression analysis to assess the risk factors for development of AKI
Discussion
In the present study, the incidence of AKI in PICU was 26.1%. This was comparable to Krishnamurthy et al where incidence was 25.1% [13]. It was high compared to other studies conducted in developed countries such as Schneider et al where incidence was 10% which used only serum creatinine to define AKI and not change in eCCl [14]. However it was lower than reported figure of 82% according to Akan-Arican et al, in which all patients had respiratory failure and were in receipt of mechanical ventilation [15]. This difference can be explained by heterogeneity of patient population, regional differences and sample size can explain this difference.
AKI stratum R, I, F was diagnosed in 60.7%, 28.6% and 10.7% OF AKI cases. The results are comparable to Mehta et al. Maximum number of AKI patients were in Stratum R. Altogether there was progression in grades in 76 cases, maximum progression was from 'No AKI' to stage R. Amongst the three pRIFLE stages maximum progression was seen in stage R to stage I. This was similar to results of both Hoste et al and Hui et al which also showed maximum progression to stage I from stage R [16,17] Pediatric RIFLE criteria use both eCrCl and urine output criteria for classification of AKI stages. In this study urine output criteria was applied only to those patients who were catherized for accurate measurement of urine output. Of the cases for whom urine output criteria was applied there was matching in 77% between urine output and eCrCl criteria. Akcan-Arikan et al and Krishnamurthy et al observed matching of 35% and 37% between urine output and serum creatinine criteria comparable to the present study [13,15]. It was observed that there is an increasing trend in matching between the urine output and eCrCl with progression of stage.
The maximum number, 28% of AKI patients were below 1 year in our study which was comparable to Mehta et al. This shows that patients with AKI were younger than those without AKI.
The etiology of AKI varies from developed and developing countries. While sepsis, glomerulonephritis, HUS and ATN predominate in developing countries, these are replaced by major surgery, haemato-oncological complications, nephrotoxic drugs and pulmonary failure as cause of AKI. In this study too infections contributed to majority of AKI cases. Amongst infections dengue (30%) was the most common etiology associated with AKI, followed by sepsis (21.9%) and then pneumonia (17.9%). Tropical febrile illnesses have been associated with AKI. Dengue is a tropical febrile illness that is common in this part of country. Dengue constituted the majority of cases. The next common etiology was sepsis. According to both Krishnamurthy et al and Mehta et al sepsis was the most common etiology associated with AKI. There is geographical variation in the etiology. There were no post renal etiologies detected in this study. This could be probably attributed to the post renal causes run a chronic course with progressive deterioration of renal function and also that their detection is more frequent in pediatrics wards than in PICU.
Prerenal causes account for majority of the AKI (68%) as renal diseases were excluded from the study. In our study risk factors for AKI were hypotension, nephrotoxic drugs, sepsis and Need for Ventilation. Hypotension was found in 75.3% of patients with AKI (p<0.001). Nephrotoxic drugs were associated with 42.1% of AKI cases (p<0.001). Sepsis was present in 21.9% of AKI cases (p<0.001). Need for mechanical ventilation was there in 20.2% cases (p<0.001). This is comparable with Mehta et al and Mendonca et al [18].
The potential limitation of this study is the use of an assumed baseline eCrCl. Furthermore urine output criteria could not be applied to all patients as only patients who were catheterized were included for urine output criteria.
Conclusion
AKI incidence in high in children admitted to PICU. AKI commonly associated with severe dengue, sepsis and pneumonia. It is amenable to treatment provided early diagnosis and prompt treatment. Early identification requires uniform definition and staging system to guide intervention. This study supports use of the pRIFLE score as an easy and simple tool for identification and classifying AKI.
References
- Ravindra Mehta, J Cerda. International Society of Nephrology’s 0by25 Initative for acute kidney injury: a human rights case for nephrology. The Lancet 2015.
- PaweenaSusantitaphong, Dinna N. Cruz, Cerda J, Maher Abulfaraj, Fahad A, et al.,, For the Acute Kidney Injury Advisory Group of the American Society of Nephrology. ‘World Incidence of AKI: A Meta-Analysis. ‘Clin J Am SocNephrol 2013; 8: 1482-1493.
- Andreoli SP. Acute kidney injury in children, PediatrNephrol. 2009;24:253-263.
- Askenazi DJ, Feig DI, Graham NM, Hui-Stickle S, Goldstein SL. 3-5 year longitudinal follow-up of pediatric patients after acute renal failure. Kidney Int. 2006;69:184-189.
- Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure: Definition, outcome measures, animal models, fluid therapy and information technology needs: The Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204-12.
- Lameire N, Van Biesen W, Vanholder R. The changing epidemiology of acute renal failure. Nat Clin PractNephrol 2; 2006:364-377.
- Cerdá J, Bagga A, Kher V, Chakravarthi RM. The contrasting characteristics of acute kidney injury in developed and developing countries. Nat Clin PractNephrol. 2008;4:138-153.
- Cerda J, Lameire N, Pannu N, Uchino S, Wang H, et al. Epidemiology of acute kidney inury. Clin J AM SocNephrol. 2008;3:881-886
- Mehta P, Sinha A, Sami A, Hari P. Incidence of Acute Kidney Injury in Hospitalized Children.
- Bowers LS, Wong ET. Kinetic serum creatinine assay II. A critical analysis and review. Clin Chem. 1980;26:555-561.
- Goldstein B, Giroir B, Randolph A.International Pediatric Sepsis Consensus Conference: Definitions for sepsis and organ dysfunction in Pediatrics. PediatrCrit Care Med. 2005;6:2-8.
- Basu RK, Prasad DP, Wong H, Wheeler DS. An update and review of acute kidney injury in pediatrics. PediatrCrit Care Med. 2011;12:339-347.
- Krishnamurthy S, Mondal N, Narayanan P, Biswal N, Srinivasan S, et al., Incidence and etiology of acute kidney injury in southern india. Indian J Pediatr. 2013;80:183-189.
- Schneider J, Khemani R, Grushkin C et al., Serum creatinine as stratified in the RIFLE score for acute kidney injury is associated with mortality and length of stay for children in the pediatric intensive care unit. Crit Care Med 2010; 38:933-939.
- Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, et al., Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int. 2007;71:1028-1035.
- Hoste EA, Clermont G, Kersten A, Venkataraman R, Angus DC, De Bacquer D, et al., RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: A cohort analysis. Crit Care. 2006;10:R73-82.
- WF Hui, Chan W, Miu TY et al. acute kidney injury in the pediatric intensive care unit: identification by modified RIFLE criteria. Hong Kong Med J.2013; 19:13-19.
- De Mendonça, Arnaldo, et al. "Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score." Intensive care medicine 2000;915-921.