Current Pediatric Research
International Journal of Pediatrics
Implementation of Case Based Learning (CBL) approach in paediatrics, a prospective observational study
Minakshi Bhat, Varsha Mane*, Karuna, Shlani S, Sheetal B, Chandrashekhar Koli
Department of Paediatrics, Terna Medical College, Nerul, Navi Mumbai, India
- Corresponding Author:
- Varsha Mane
Department of Paediatrics,
Terna Medical College,
Nerul,
Navi Mumbai,
India
E-mail: drvarshacardio@gmail.com
Received: 11-Sep-2024, Manuscript No. AAJCP-24-147742; Editor assigned: 13-Sep-2024, AAJCP-24-147742 (PQ); Reviewed: 26-Sep-2024, QC No. AAJCP-24-147742; Revised: 11-Nov-2024, Manuscript No. AAJCP-24-147742 (R); Published: 18-Nov-2024, DOI:10.35841/0971-9032.28.10.2359-2367
Citation:Bhat M, Varsha M, Karuna, et al. Implementation of Case-Based Learning (CBL) approach in paediatrics, a prospective observational study. Curr Pediatr Res 2024;28(10):2359-2367.
Aims and objectives: 1) To assess and compare the performance of students before and after didactic lecture and case based learning. 2) To assess the perception of students and teachers about CBL by pre-validated questionnaire using a five-point scale.
Materials and methods: The study conducted in the department of paediatrics, Terna medical college, Nerul, Navi Mumbai, III year MBBS students of our college participated in the study. They were divided into two batches (A and B) by simple random sampling. These two batches were exposed to didactic lecture and CBL respectively in topic 1 and then crossover was done in second week for the topic 2. Topic 1 was nephrotic syndrome and topic 2 was thalassemia. The student’s knowledge before and after both the sessions was assessed by pre and post-test questionnaire. Perception of students and teachers about CBL was assessed by pre-validated questionnaire using a five-point scale.
Evaluation plans: Outcome was measured by comparison of pre-test and post-test scores using “Paired t tests” in both groups in each session separately for topic 1 and 2. Post test scores in CBL group and didactic lecture group was compared by “Unpaired t test”. Students and faculty responses on perception about CBL on 5-point Likert scales were analyzed using percentages.
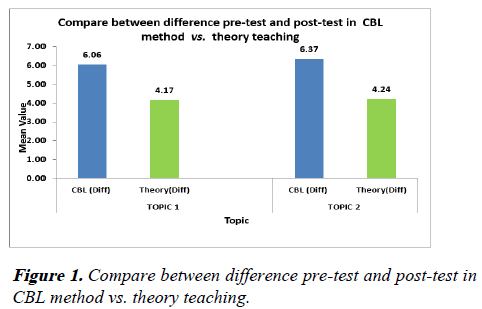
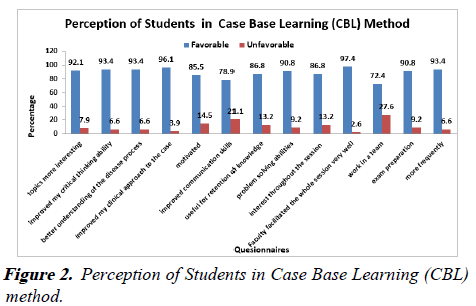
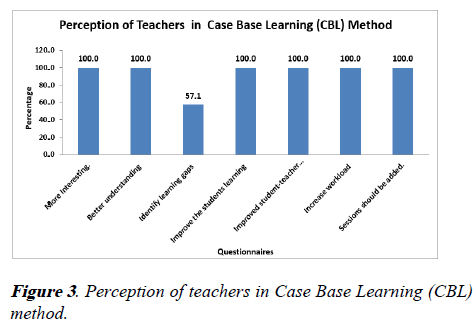
Results: We compared between differences of pre-test and post-test in Case Base Learning (CBL) method vs. theory teaching. The mean difference for two methods for both topics were statistically significant with p value of <0.001. More than 90% of students perceived CBL sessions more interesting, helpful in improving critical thinking ability, problem solving abilities and communication skills whereas 100% teachers perceived CBL sessions helpful in making subject interesting, improving learning abilities, student-teacher interaction and better understanding.
Conclusion: Considering the positive perception of the students and the faculty, in resource-intensive settings CBL can be used in combination with traditional didactic lecture method for promoting critical thinking and problem-solving abilities of the students. CBL is an effective tool for imbibing clinical skills during paediatrics learning.
Keywords
Case based learning, Critical thinking, Problem-solving abilities, Didactic lecture, Questionnaire, Perception.
Introduction
There are various methods of learning in medical science each having its own advantages and disadvantages. In India, the undergraduate medical education is primarily lecture-based, though many teaching bodies are evaluating and applying innovative teaching interventions. In its vision 2015 document, the MCI has promoted early clinical exposure and emphasized on five roles of a doctor, including those of a clinician, a lifelong learner, a leader and member of the health care team. To achieve these needs, Case Based Learning (CBL) seems to be a promising teaching method [1]. CBL is an interactive, student-centred, instructor-led learning approach that is closely related to PBL. This innovative learning approach was first applied in medical education by the anatomy department of a medical school in Newfoundland, Canada [2].
There have been many studies to evaluate the small-group CBL learning. However, there is scope of further research on the educational benefits of CBL in a large group setting. This study was undertaken to introduce the students to an alternative method of learning (CBL) compared with the traditional one used (Didactic Lecture (DLs)) in a large classroom setting, to assess the students’ performance and perception of students and faculties of paediatrics regarding the same.
Objectives
• To study the implementation of Case-Based Learning (CBL) approach as a teaching-learning method in the subject of paediatrics.
• To study the perception of III-year MBBS students about CBL as a teaching learning method in paediatrics.
• To study the perception of teachers about CBL as a teaching learning method in paediatrics.
• To study the perception of teachers about CBL as a teaching learning method in paediatrics.
Materials and Methods
Study design: Prospective interventional study.
Study duration: 4 months.
Study setting: Department of paediatrics, Terna Medical College, Nerul.
Study sample: A batch of 3rd MBBS part II students (100).
Sampling technique: Simple random sampling
The study was conducted in the department of paediatrics in Terna Medical College, Nerul, Navi Mumbai. III-year MBBS part II students at our college participated in the study. After obtaining ethics committee approval and written informed consent from students, the willing students were divided into two batches (A and B). These two batches were exposed to didactic lecture and CBL respectively in topic 1 and then crossover was done in second week for the topic 2. Topic 1 was nephrotic syndrome and topic 2 was thalassemia. The student’s knowledge before and after both the sessions was assessed by pre and post-test questionnaire pre-validated by peer review.
Topic 1
Nephrotic case: A 3-year-old male toddler weighing 15 kg presented with a history of high grade continuous fever associated with high grade fever with running nose and cough. The patient had cough with whitish colour sputum not foul smelling. Swelling over face was present which initially started around peri-orbital (which is more during morning) and gradually progressed to legs which decreases by evening. The toddler had decreased urine output (oligouria). On examination pitting type of oedema was present over lower limbs and swelling over face was present. Based on these clinical presentations, nephrotic syndrome was suspected and specific laboratory testing was performed to establish diagnosis.
The urine dipstick indicated 3+ proteinuria and no hematuria. Blood test showed hypoalbuminemia of 2 g/dl (reference interval of 3.5 to 5.5 g/dl). The urine protein creatinine ratio was 3.5. This was suggestive of Nephrotic syndrome. Complete blood count showed normal leukocytes count with high lymphocytes count. CRP was negative and mantoux test was negative. Thus prednisolone was started along with high protein diet. Urine output and blood pressure was monitored. The periorbital edema and leg swelling reduced over time. Serum cholesterol increased and urine proteins reduced over 10 days.
Topic 2
Thalasemia case: 8-years-old male child with anemia, jaundice and fatigue, specific hemolytic facial features diagnosed with anemia at 8 months which requires frequently (every 2 months) blood transfusions, started on chelation medicine desferroxamine from 6 years to 4 years of age, being stunted and underweight with hepatosplenomegaly. Splenectomy was the treatment plan. Complete blood picture, peripheral smear, Hb electrophoresis were characteristic of thalassemia. Blood film showed microcytosis, target cells, nucleated red cells, and anisopoikilocytosis. There was reduced hemoglobin level (<7 g/dL) and very low MCH (<20 pg). HbEP was showing low HbA2 and high Hb F.
Perception of students and faculty about CBL was assessed by pre-validated questionnaire using a five-point Likert scale. This perception questionnaire was based on recall (10%), comprehension (30%), analysis (30%) and application of clinical skills (30%). The five point Likert scale responses included grades of strongly agree, agree, neutral, disagree and strongly disagree. Favourable response included agrees and strongly agree whereas unfavourable response included neutral, disagree and strongly disagree.
Evaluation plans: Outcome was measured by comparison of pre-test and post-test scores using “paired t tests” in both groups in each session separately for topic 1 and 2. Post test scores in CBL group and didactic lecture group was compared by “unpaired t test”. Students and faculty responses on perception about CBL on 5-point Likert scales were analyzed using percentages.
Results
During the assessment of topic 1 by CBL, the mean scores of pre-test and post-test were 5.3 and 11.36, while topics 1 by didactic lecture, the mean scores of pre-test and post-test were 4.83 and 9 (Table 1). This showed statistically significant difference with p value of <0.001. During the assessment of topic 2 by CBL, the mean scores of pre-test and post-test were 4.6 and 10.98 while topic 2 by didactic lecture, the mean scores of pre-test and post-test were 5.44 and 9.68 (Table 2). Both showed statistically highly significant difference 0.1% level i.e., P<0.001.
| Method | N | Mean | SD | Median | Wilcoxon Signed rank Test | P-value | Sig. at 5% level |
|---|---|---|---|---|---|---|---|
| CBL | |||||||
| Pre Test | 40 | 5.3 | 1.497 | 5.5 | 5.449** | 0.000 | Yes |
| Post Test | 40 | 11.36 | 1.5851 | 11.5 | |||
| Theory | |||||||
| Pre Test | 41 | 4.83 | 1.6756 | 4.5 | 5.489** | 0.000 | Yes |
| Post Test | 41 | 9 | 1.6283 | 9 | |||
Note:** Statistically highly significant 0.1% level i.e. P<0.001.
Table 1. Assessment of Case Base Learning (CBL) method and theory teaching: Topic 1 (Nephrotic syndrome).
| Method | N | Mean | SD | Median | Wilcoxon Signed rank Test | P-value | Sig. at 5% level |
|---|---|---|---|---|---|---|---|
| CBL | |||||||
| Pre Test | 41 | 4.61 | 1.0637 | 4.5 | 5.607** | 0.000 | Yes |
| Post Test | 41 | 10.98 | 1.294 | 11 | |||
| Theory | |||||||
| Pre Test | 40 | 5.44 | 1.4901 | 5 | 5.5556** | 0.000 | Yes |
| Post Test | 40 | 9.68 | 1.2483 | 10 | |||
Note:** Statistically highly significant 0.1% level i.e. P<0.001.
Table 2. Assessment of Case Base Learning (CBL) method and theory teaching: Topic 2 (Thalassemia).
We compared between difference of pre-test and post-test in Case Base Learning (CBL) method vs. theory teaching. The mean of difference of all 40 students of CBL approach for topic 1 was 6.0627 whereas that for topic 2 was 6.3659. The mean of difference of all 41 students of lecture approach for topic 1 was 4.1707 whereas that for topic 2 was 4.2375. The mean difference between CBL and lecture methods for topic 1 and topic 2 were 1.89 and 2.12 respectively (Table 3 and Figure 1). Thus, mean difference for two methods for both topics were statistically significant with p value of <0.001. More than 90% of students perceived CBL sessions more interesting, helpful in improving critical thinking ability, problem solving abilities and communication skills whereas 90.8% students perceived CBL sessions are helpful for exam preparation (Figure 2 and Table 4). Perception of teachers in Case Base Learning (CBL) method-100% teachers perceived CBL sessions helpful in making subject interesting, improving learning abilities, student-teacher interaction and better imbibing of clinical skills. 87.5% teachers perceived CBL helpful to identify learning gaps in students (Table 5 and Figure 3).
| Method | Mean | SD | Mean Diff | Independent T test | P-value | Sig. at 5% level |
|---|---|---|---|---|---|---|
| Topic 1 (Nephrotic syndrome) | ||||||
| CBL (Diff) (n=40) | 6.0625 | 2.0575 | 1.8918 | 4.122** | 0.000 | Yes |
| Theory (Diff) (n=41) | 4.1707 | 2.0725 | ||||
| Topic 2 (Thalassemia) | ||||||
| CBL (Diff) (n=41) | 6.3659 | 1.1293 | 2.1284 | 8.007** | 0.000 | Yes |
| Theory (Diff) (n=40) | 4.2375 | 1.2608 | ||||
Note: ** Statistically highly significant 0.1% level i.e. P<0.001.
# Diff=Difference between pre-test and post test
Table 3. Compare between difference pre-test and post-test in Case Base Learning (CBL) method vs. theory teaching: Topic 1 (Nephrotic syndrome) and topic 2 (Thalassemia).
Improvement of students score in CBL method is better than theory method in both topic 1 and 2.
| Perception | Max Score | Favorable | % | Unfavorable | % | Total |
|---|---|---|---|---|---|---|
| Students | ||||||
| CBL sessions made topics more interesting | 76 | 70 | 92.1 | 6 | 7.9 | 76 |
| CBL sessions improved my critical thinking ability | 76 | 71 | 93.4 | 5 | 6.6 | 76 |
| CBL helped me in better understanding of the disease process | 76 | 71 | 93.4 | 5 | 6.6 | 76 |
| CBL improved my clinical approach to the case | 76 | 73 | 96.1 | 3 | 3.9 | 76 |
| CBL motivated me for self-directed learning | 76 | 65 | 85.5 | 11 | 14.5 | 76 |
| CBL improved my communication skills | 76 | 60 | 78.9 | 16 | 21.1 | 76 |
| CBL session proved useful for retention of knowledge | 76 | 66 | 86.8 | 10 | 13.2 | 76 |
| CBL improved my problem solving abilities | 76 | 69 | 90.8 | 7 | 9.2 | 76 |
| CBL held my interest throughout the session | 76 | 66 | 86.8 | 10 | 13.2 | 76 |
| Faculty facilitated the whole session very well | 76 | 74 | 97.4 | 2 | 2.6 | 76 |
| CBL encouraged me to work in a team | 76 | 55 | 72.4 | 21 | 27.6 | 76 |
| CBL sessions are helpful for exam preparation | 76 | 69 | 90.8 | 7 | 9.2 | 76 |
| CBL sessions should be held more frequently | 76 | 71 | 93.4 | 5 | 6.6 | 76 |
Table 4. Perception of students in Case Base Learning (CBL) method: Opinion.
| Perception | Max Score | Favorable | % | Unfavorable | % | Total |
|---|---|---|---|---|---|---|
| Teacher | ||||||
| CBL sessions will make the subject more interesting. | 7 | 7 | 100.0 | 0 | 0 | 7 |
| Will help in better understanding of the disease process. | 7 | 7 | 100.0 | 0 | 0 | 7 |
| Will help identify learning gaps in students. | 7 | 4 | 57.1 | 3 | 42.9 | 7 |
| Will improve the students learning abilities. | 7 | 7 | 100.0 | 0 | 0 | 7 |
| Will lead to improved student-teacher interaction. | 7 | 7 | 100.0 | 0 | 0 | 7 |
| Will increase workload on faculty. | 7 | 7 | 100.0 | 0 | 0 | 7 |
| More such sessions should be added. | 7 | 7 | 100.0 | 0 | 0 | 7 |
Table 5. Perception of teachers in Case Base Learning (CBL) method: Opinion.
Discussion
Discussion on implementation on CBL
Paediatrics is a clinical medical speciality and learning the subject by traditional method of lecture based learning imparts inadequacy of clinical knowledge. Inculcating case based learning approach helps to add clinical aspects to cognitive domain of students.
Case-based teaching was first applied at Harvard Law School in 1870 and later adopted by Harvard Business School in 1920. For medical education, it was first applied by the anatomy department of a medical school in Newfoundland [3-5]. The Medical Council of India has also recommended the introduction of Case-Based Learning (CBL) in basic medical subjects [6,7]. CBL is defined as an inquiry structured learning experience utilizing live or simulated patient cases to solve, or examine a clinical problem, with the guidance of a teacher and stated learning objectives. Advantages of using CBL include more focusing on learning objectives, flexibility on the use of the case, and ability to induce a deeper level of learning by inducing more critical thinking skills [8]. A 2011 article in critical care medicine demonstrated the utility of both simulators and CBL on behaviours in critical situations of critical care teams of physicians and nurses [9]. In our study, questions specifically focusing on clinical skills like edema, pallor, ascites, hemolytic facies, hepatosplenomegaly, short stature were included in questionnaire. In the pre-test and posttest questionnaire answered by students CBL batch answered more questions based on clinical skills correctly compared to the batch of didactic lecture. Also, during perception assessment CBL batch students emphasized on clinical skills well understood in CBL than through didactic lecture method.
Palliative care 21 and primary care 51,59 articles also reported on using a CBL course for learning with physicians and nurses. An article from the United Arab Emirates discussed how CBL better prepared participants for critical situations as well as basic primary care [10-12]. Another paper from Germany describes initiation of a CBL curriculum for medical students and lists the pitfalls in establishing this curriculum [13]. This study was initially planned as a case-control study of lecture versus CBL format with crossover. Comparing lecture and CBL: The improved attendances of students in our CBL sessions show the students were motivated and interested to learn through CBL. The significant increase in attendance of students in CBL classes is similar to the CBL study reported by Klegeris and Hurren 22 and Smith and Cook [14,15]. The difference between scores of both methods for both topics were statistically significant with p value of <0.001. The mean difference between scores for CBL method for both the topics were higher than the mean difference for didactic lecture method and it was statistically significant.
Kaur et al., showed there was significant difference (P=.008, t=2.65) in attendance between the 2 groups (CBL vs. DL) whereas there was no significant difference (P=.98) between the average marks scored by the students in the CBL and DL methods explained by the t-unpaired test. However, on applying the t-test on the detailed mark list (based on the type of questions asked), it was found that there was significant increase in marks obtained by students taught by CBL regarding questions which involved critical thinking (than the DL method). On the contrary, the knowledge-based questions showed significantly better results in the DL 9 didactic lecture) method than in the CBL method. Thus, there was no significant increase in marks in studies by Kaur et al., and similar results were found in Michael et al. [16,17]. This preliminary data suggests there would be benefit to continuing and introducing more interactive case-based tutorials in the medical microbiology course.
Kolahdouzan M et al., showed in his study in surgery interns that CBT and flipped classroom improved students’ learning and the quality of teaching and students were more satisfied with this method in comparison with the lecture method [18].
Perception of students
By and large, our data demonstrated that the majority of the students not only accepted this innovative technique but were also satisfied about the quality of cases discussed in the CBL. More than 90% perceived CBL sessions more interesting, helpful in improving critical thinking ability, problem solving abilities and communication skills whereas 90.8% students perceived CBL sessions are helpful for exam preparation. Similar projects showed following results. In a comparative study conducted by Gupta et al., 17 76% of the students found the CBL sessions to be better than theory lectures compared with our study [19]. In a maxillofacial radiology course, Kumar et al., reported that the majority of students felt that case-based instruction helped them learn course contents in a more comprehensive manner and increased their knowledge of radiographic interpretation [20]. Yoo et al., examined the effects of CBL on learning motivation in nursing students and found that it was significantly higher in the CBL group than in the non-CBL one [21]. Ciraj et al., reported that student communication skills and ability to work within a team were significantly improved due to CBL implementation in a microbiology course [22]. Our study perception was different from findings of Kaur et al., where students mentioned some drawbacks of CBL of slow lectures and greater efforts required in the class, whereas many students suggested increasing the number of CBL sessions, asked for more cases, and were quite excited to answer the problems. Few studies have shown satisfactory response of CBL by students IN dermatology, cytopathology and OBGY department.
Interactive case-based teaching improved learning outcomes and increased student satisfaction in a dermatology program [23]. The authors were able to show significant differences between students taking the case-based approach versus the standard lecture course. Dermatology study had more participants (N>200), incorporated bedside teaching and used more sessions. In another study, an electronic, interactive, casebased cytopathology component was found to be useful in second year medical student teaching [24]. More reliable, however, are the studies that have shown that students enjoy CBL and are better able to connect theory to clinical practice as well as improvements in the engagement of students, with CBL fostering more active and collaborative learners [25,26]. Massonetto et al., in his study in OBGY teaching programme, concluded that the insertion of clinical cases and practical classes into the traditionally theoretical course was the decisive factor in students' perception that the lessons had improved [27].
Perception of faculties
Amongst the faculty perceptions, student enthusiasm and active participation was more in case based approach in contrast to routinely held tutorials where only few students come prepared and interact. 100% teachers perceived CBL sessions helpful in making subject interesting, improving learning abilities, student-teacher interaction and better understanding whereas 57.5% teachers perceived CBL helpful to identify learning gaps in students. The faculty feedback was positive and so wanted to incorporate CBL for other important topics and combine it with traditional lectures methods, which are similar to the findings concluded by Dube et al. [28]. Considering the positive perception of the students and the faculty, in resource-intensive settings CBL can be used in combination with traditional didactic lecture method for promoting critical thinking and problem-solving abilities of the students.
Application of CBL in paediatric
There are number of clinical skills involved in paediatrics where CBL can play an important role. Clinical skills involved in physical examination of neonates, children and adolescents are taught in ward rounds or bedside teaching. Normal and abnormal findings of general examination and systemic examination are better learnt on specific cases. For instance, whether the fontanel is normal, wide open or bulging can be appreciated only when taught on specific cases like normal, rickets or hydrocephalus respectively. In this aspect, CBL helps integrate basic science with clinical sciences. Instructor led learning approach facilitates in such learning of clinical skills.
Respiratory findings of tracheal tug, stridor, intercostal retractions, intercostal retractions and cardiac findings like bulging precordium, hyperdyanamic apex, location of apex beat, parasternal heave, various murmur, clicks and rubs can be learnt only by attending to many pathological cases. All these clinical features are better learnt if CBL approach is added to the didactic lecture. Hypertonia, exaggerated reflexes, contractures, pseudobulbar palsy, persistent primitive reflexes can be well demonstrated on a case of cerebral palsy during CBL method. Various grades of hepatosplenomegaly are appreciated through spectrum of cases like hemolytic anemias, malignancy and infections involving-dengue, malaria, typhoid, infectious mononucleosis. Diagnostic clinical skills like intravenous, central line catheter insertion, pleural tap, ascitic tap, lumbar puncture can be better understood with case based approach apart from PICU rounds and bedside teaching. These skills are learnt effectively if knowledge and skills are inserted and conceptualised in relevant real life and problem based situations.
Spectrum of pathology in various diseases from the result of these invasive diagnostic skills and their correlation with clinical findings of respective cases can be well perceived by students by case based approach. This includes clinical spectrum of bacterial vs. viral infection on pleural effusion, ascites, meningitis and their correlation with specific pathological findings on fluid reports of pleural tap, ascitic tap and CSF respectively. It stimulates thinking, reasoning and self-directed learning. On the other hand, CBL is mandatory in clinical skills involved in management of certain paediatrics diseases like intramuscular, intravenous injections, ICU care, therapeutic management of respiratory support, weaning of mechanical ventilation and extubation.
An integral part of paediatric management is assessment of growth, nutrition, development and vaccination. Growth assessment needs accurate measurement of growth parameters like weight, height, mid upper arm circumference, their comparison with normal standards. Developmental assessment needs accurate assessment of current development in all domains (fine motor, gross motor, adaptive, language and social), comparing with normal range and analysing the behaviour patterns. All these skills are facilitated by CBL approach.
Teachers are also reflecting upon their learning process through CBL approach by formulating and introducing cases to students. Understanding the need of vaccination according to the national schedule of vaccines in each child with application, indication and contraindications is utmost important in paediatrics. All the vaccines related skills of intramuscular, intradermal, subcutaneous vaccines and need of special ones in specific diseases can be well demonstrated with case based approach only.
The study needs to be carried forward to see the intermediate and long-term outcomes.
Pros and cons of CBL
Self: Explored a new TL method which was welcome by all students and faculty.
Dept.: Faculties were excited to include CBL method in our further teaching programme henceforth in paediatric department of Terna Medical College.
Institute: Other clinical departments also adopted this CBL method. CBL encourages independent learning and deeper understanding of a particular topic and promotes life-long learning. CBL changes the teacher into a facilitator who can blend with the students, become familiar with them at a more personal level, trigger the discussion and encourage student participation [29,30].
Cons: A limitation of the current study is that only two cohorts of students who were exposed to the session were examined and they participated in the sessions somewhat differently. Inclusion of additional cohorts of students who participated in the tutorial would be beneficial. Few studies have mentioned the challenges of CBL implementation. Nair SP et al., has discussed the effectiveness of CBL, we must remember that it requires motivated and trained faculty, validated case scenarios, infrastructural and logistical support and most important, the time for planning and preparation [31]. Nordique J et al., in his study found the implementation of CBL was not satisfactory and focussed on exposure of the weaknesses of the implementation process, the misalignment between CBL and the reigning teaching and learning regime, and promotion of the future use of the checklist for future successful implementation of CBL in any surgical undergraduate curriculum. At the same time, CBL utilizes patients for generating interest and promoting better contextual understanding of the pre- and para-clinical individuals, which may otherwise seem dry and boring. The long-term outcomes of CBL also need to be evaluated.
Study limitations
Limitation of the current study is that only two cohorts of students who were exposed to the session were examined and crossover was assessed. Additional cohorts inclusion would have been beneficial. Different faculties took CBL and didactic lecture on the same topic which may change the efficiency of each method of teaching.
Future implications
It will be a challenge to implement the new curriculum across India, from training the faculty to adopting the novel Teaching- Learning (TL) methods, but most importantly to attempt a change in the conventional mind-set of the teachers and learners. Further research is needed that includes evaluation of the performance of multiple cohorts.
Conclusion
Considering the positive perception of the students and the faculty, in resource-intensive settings CBL can be used in combination with traditional didactic lecture method for promoting critical thinking and problem-solving abilities of the students. CBL is an effective tool for imbibing clinical skills during paediatrics learning.
References
- Williams B. Case based learning a review of the literature: Is there scope for this educational paradigm in prehospital education?. Emerg Med J. 2005;22(8):577-81.
[Crossref] [Google Scholar] [PubMed]
- Thistlethwaite JE, Davies D, Ekeocha S, et al. The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No. 23. Med Teach. 2012;34(6):e421-44.
[Crossref] [Google Scholar] [PubMed]
- Bereiter C, Scardamalia M. Cognitive coping strategies and the problem of “inert knowledge”. InThinking and learning skills 2013:65-80.
- Garvin D. Making the case: Professional education for the world of practice in Harvard Magazine. 2003:56.
- Scott TM. A case based anatomy course. Med Educ. 1994;28(1):68-73.
[Crossref] [Google Scholar] [PubMed]
- Medical Council of India. Regulations on graduate medical education, 1997. Notification, Gazette of India, Part III, Sect. 4. 1997. Amended Upto Ma, 2018.
- National Medical Commission. Competency based undergraduate curriculum for the Indian Medical Graduate. 2023.
- Bi M, Zhao Z, Yang J, et al. Comparison of case-based learning and traditional method in teaching postgraduate students of medical oncology. Med Teach. 2019;41(10):1124-28.
[Crossref] [Google Scholar] [PubMed]
- Frengley RW, Weller JM, Torrie J, et al. The effect of a simulation-based intervention on the performance of established critical care unit team. Crit Care Med. 2011;39(12):2605–11.
[Crossref] [Google Scholar] [PubMed]
- Ellman MS, Schulman-Green D, Blatt L, et al. Using online learning and interactive simulation to teach spiritual and cultural aspects of palliative care to interprofessional students. J Palliat Med. 2012;15(11):1240–47.
[Crossref] [Google Scholar] [PubMed]
- Pearson D, Pandya H. Shared learning in primary care: Participant’s views of the benefits of this approach. J Interprof Care. 2006;20(3):302–13.
[Crossref] [Google Scholar] [PubMed]
- Revel T, Yussuf H. Taking primary care continuing professional education to rural areas: Lessons from the United Arab Emirates. Aust J Rural Health. 2003;11:271–76.
[Crossref] [Google Scholar] [PubMed]
- Nordquist J, Sundberg K, Johansson L, et al. Case-based learning in surgery: Lessons learned. World J Surg. 2012;36(5):945-55.
[Crossref] [Google Scholar] [PubMed]
- Klegeris A, Hurren H. Impact of problem-based learning in a large classroom setting: Student perception and problem-solving skills. Adv Physiol Educ. 2011;35:408-15.
[Crossref] [Google Scholar] [PubMed]
- Smith M, Cook K. Attendance and achievement in problem-based learning: The value of scaffolding. Interdisc J Prob Based Learn. 2012;6:129-52.
- Kaur G, Rehncy J, Kahal KS, et al. Case-based learning as an effective tool in teaching pharmacology to undergraduate medical students in a large group setting. J Med Educ Curric Dev. 2020;7.
[Crossref] [Google Scholar] [PubMed]
- Michel MC, Bischoff A, Zu Heringdorf M, et al. Problem vs. lecture-based pharmacology teaching in a German medical school. Naunyn Schmiedebergs Arch Pharmacol. 2002;366:64-8.
[Crossref] [Google Scholar] [PubMed]
- Kolahdouzan M, Mahmoudieh M, Rasti M, et al. The effect of case-based teaching and flipped classroom methods in comparison with lecture methods on learning and satisfaction of internship students in surgery. J Educ Health Promot. 2020;9:256.
[Crossref] [Google Scholar] [PubMed]
- Gupta K, Arora S, Kaushal S. Modified case based learning: Our experience with a new module for pharmacology undergraduate teaching. Int J Appl Basic Med Res. 2014;4:90-4.
[Crossref] [Google Scholar] [PubMed]
- Kumar V, Gadbury-Amyot CC. A case-based and team-based learning model in oral and maxillofacial radiology. J Dental Educ. 2012; 76:330-37.
[Google Scholar] [PubMed]
- Yoo MS, Park JH, Lee SR. The effects of case-based learning using video on clinical decision making and learning motivation in undergraduate nursing students. J Korean Acad Nursing. 2010;40:863-71.
[Crossref] [Google Scholar] [PubMed]
- Ciraj AM, Vinod P, Ramnarayan K. Enhancing active learning in microbiology through case-based learning: Experiences from an Indian medical school. Indian J Pathol Microbiol 2010; 53:729–33.
[Crossref] [Google Scholar] [PubMed]
- Ochsendorf FR, Boehncke WH, Sommerlad M, et al. Interactive large-group teaching in a dermatology course. Med Teach. 2006;28:697-701.
[Crossref] [Google Scholar] [PubMed]
- Steinberg DM, Chan TY, Freedman JA, et al. Teaching cytopathology to second-year medical students. Acta cytologica. 2002;46(3):481-89.
[Crossref] [Google Scholar] [PubMed]
- Hakkarainen P, Saarelainen T, Ruokamo H (2007) Towards meaningful learning through digital video supported, case based teaching. Australas J Educ Technol. 2007;23(1).
- Hansen WF, Ferguson KJ, Sipe CS, Sorosky J. Attitudes of faculty and students toward case-based learning in the third-year obstetrics and gynecology clerkship. Am J Obstet Gynecol. 2005;192(2):644–47.
[Crossref] [Google Scholar] [PubMed]
- Massonetto JC, Marcellini C, Assis PS, et al. Student responses to the introduction of case-based learning and practical activities into a theoretical obstetrics and gynaecology teaching programme. BMC Med Educ. 2004;4:1-7.
[Crossref] [Google Scholar] [PubMed]
- Dube SP, Ghadlinge MS, Mungal SU, et al. Students’ perception towards the problem based learning. IOSR-JDMS. 2014;13:49-53.
- Barrows HS, Tamblyn RM. Problem-based learning: An approach to medical education. Springer Publishing Company. 1980:15.
- Garvey MT, O'Sullivan M, Blake M. Multidisciplinary case based learning for undergraduate students. European J Dental Educ. 2000;4(4):165-68.
[Crossref] [Google Scholar] [PubMed]
- Nair SP, Shah T, Seth S, et al. Case based learning: A method for better understanding of biochemistry in medical students. J Clin Diagn Res. 2013;7:1576-78.
[Crossref] [Google Scholar] [PubMed]