Current Pediatric Research
International Journal of Pediatrics
Epidemiology and effect of a new variant (from alpha to delta strains) of SARS-COV-2 for children and adults.
Bibigul Doltayeva*, Altynshash Kushkarova, Parkhat Utepov, Sara Yeskerova, Akmaral Zhumadilova
Department of Pediatrics, South Kazakhstan Medical Academy, Shymkent, Kazakhstan
- Corresponding Author:
- Bibigul Doltayeva
Department of Pediatrics
South Kazakhstan Medical Academy
Shymkent
Kazakhstan
Tel: +7(777)4003374
E-mail: salta3105@mail.ru
Accepted date: 25th October, 2021
Background: Several clinical studies have demonstrated that arterial stiffness is an early indicator of cardiovascular events. Our study aimed to detect the potential cardiovascular changes using arterial stiffness parameters and compare these changes with echocardiographic aortic stiffness parameters in cancer patients treated with cardio toxic chemotherapeutics. Methods and Results: Our study is a prospective case-control study. A total of 70 subjects between the ages of 18 and 50 years were included into our study. 30 of them were newly diagnosed cancer patients and 40 were age and sex matched control group. Baseline oscillometric arterial and echocardiographic aortic stiffness parameters were measured in all patients. In cancer patients, all of these parameters were measured again one month after chemotherapy protocol was completed. Mean age of the cancer patients was 41.4 ± 5.9 years and mean age of the control group was 39.6 ± 6.6 years (p=0.258). Before chemotherapy, arterial and aortic stiffness parameters were similar between the study and the control groups. After chemotherapy, oscillometric pulse wave velocity parameter increased compared to the control group and to the pre-chemotherapy values (p=0.004 and p<0.001, respectively). After chemotherapy, augmentation index parameter increased compared to the control group (p=0.013). On the other hand, no difference was detected between the groups in terms of echocardiographic aortic stiffness parameters. Conclusion: In newly diagnosed cancer patients treated with cardio toxic chemotherapeutics, considerable impairment occurs in some of the oscillometric arterial stiffness parameters while there is no substantial effect on echocardiographic aortic stiffness. Arterial stiffness parameters in these patients might be useful in evaluating subclinical cardiovascular damage.
Keywords
Cardiotoxicity, Chemotherapy, Cancer, Arterial stiffness, Pulse wave velocity.
Introduction
The clinical impact of the new SARS-COV-2 lineage B.1.1.7 on children and young people (aged 18 years or younger) regarding acute respiratory SARS-COV-2 is yet to be fully defined [1]. Media reports of increases in admissions to hospital and more serious illness in children and young people have resulted in public confusion and implicated the B.1.1.7 variant as a more pathogenic infection within this group [1,2]. This uncertainty has necessitated a public statement from the royal college of pediatrics and child health [2,3]. It is important to rapidly clarify the true impact of the second wave on children and young people within the context of a high prevalence of the B.1.1.7 variant, estimated to account for 70% of infections in the London region in January [4]. Located in south London, king’s college hospital lies within an area of high disease prevalence, admitting large numbers of patients in both SARS-COV-2 waves [4]. We have previously published data pertaining to children and young people admitted during the first wave and here, we compare those data with the characteristics of children and young people admitted with acute respiratory SARS-COV-2 thus far during wave [5]. Between March 1, and May 31, 2020, 20 children and young people were admitted to king’s college hospital. Between Nov 1, 2020, and Jan 19, 2021, 60 children and young people positive for SARS-COV-2 were admitted. No significant differences were found in age, proportion of patients with comorbidities, proportion of patients from Black, Asia and minority ethnicity background or deprivation score between groups (Table 1).
| Wave 1 | Wave 2 | |
|---|---|---|
| (March 1, to May 31, 2020) | (Nov 1, 2020, to Jan 19, 2021) | |
| Number of patients | 20 | 60 |
| Age, years | 1 (0·1–11) | 6 (0·7–13) |
| Sex | ||
| Male | 9 (45%) | 40 (67%) |
| Female | 11 (55%) | 20 (33%) |
| Comorbidities | 7 (35%) | 25 (42%) |
| BAME ethnicity | 6 (46%; n=13) | 20 (42%; n=48) |
| IMD score | 28·3 (11·6–36·1) | 20·5 (14·7–32·2) |
| Clinical severity (modified WHO definition)* | ||
| Critical disease | 4 (20%) | 2 (3%) |
| Severe disease | 1 (5%) | 3 (5%) |
| Moderate disease | 5 (25%) | 8 (13%) |
| Mild disease | 8 (40%) | 27 (45%) |
| Asymptomatic or incidental findings | 2 (10%) | 20 (33%) |
| Management | ||
| Oxygen | 7 (35%) | 5 (8%) |
| Non-invasive ventilation | 3 (15%) | 2 (3%) |
| Invasive ventilation | 4 (20%) | 1 (2%) |
| Remdesivir | 1 (5%) | 4 (7%) |
| Steroids (low dose) | 0 | 5 (8%) |
| Monoclonal antibodies (casirivimab and imdevimab) | 0 | 1 (2%) |
Table 1. Aged 18 years or younger and positive for SARS-COV-2.
Disease severity necessitating oxygen therapy or ventilator support was infrequent in both waves and was lower as a proportion of total admission in the second wave than in the first. These early second wave data show that many children and young people have been admitted to hospital. This might be due to the higher prevalence of SARS-COV-2 within our local community. Indeed, the number of adult patients admitted to King’s college hospital in the second wave has also increased by about a third. Importantly, we have found no evidence of more severe disease having occurred in children and young people during the second wave, suggesting that infection with the B.1.1.7 variant does not result in an appreciably different clinical course to the original strain. These findings are in keeping with early national data. Severe acute respiratory SARS-COV-2 remains an uncommon occurrence in children and young people [6-9].
WHO encourages countries, through laboratory networks, to support and build capacity for sequencing and strain identification of viruses? National and local authorities are encouraged to continue strengthening existing SARS-COV-2 control activities, including epidemiological surveillance, strategic testing, and strengthening routine systematic sequencing of a representative sample of SARS-COV-2 isolates from across the country, where possible. A holistic response should continue to be taken against all cases of SARS-COV-2 transmission [10].
Distribution of the Alpha Version
The first case was detected in mid-September 2020 in London, in November 2020, it was confirmed in a sample taken in September during the SARS-COV-2 pandemic in the United Kingdom; the virus began to spread rapidly by mid-December and correlates with a significant increase in the number of cases of SARS - COV-2 infection in the world [11].
On February 2, 2021, public health England reported that they had found "a limited number of B. 1.1.7 VOC-202012/01 genomes with E484K mutations", which they called "Variant of concern, 202102/02" (VOC-202102/02). One of the mutations (N501Y) is also present in the beta and gamma variants [11].
A study conducted by the center for mathematical modeling of infectious diseases of the London school of hygiene and tropical medicine showed that the transmission of the alpha variant (line B. 1.1.7) is usually significantly higher than that of previously existing SARS-COV-2 variants in Denmark, Switzerland and the United States. This is due to a mutation inside the Receptor Binding Motif (RBM), which can change the recognition of antibodies and the specificity of ACE2 binding and lead to the virus becoming more infectious [12]. A Danish study showed that people infected with the B. 1.1.7 line are 64% (32%-104%) more likely to be admitted to hospitals compared to people infected with another line.
The alpha variant became dominant for: South-East England at week 48, the last week of November 2020. England in the 51st week of 2020; Great Britain in the 52nd week of 2020; Scotland and Northern Ireland in the first week of 2021; Wales in the second week of 2021; Ireland in the second week of 2021; In Bulgaria, genome sequencing showed that this variant prevails with 52.1% at week 4, and 73.4% at week 9 [13].
Delta-Coronavirus (Indian Strain)
The Indian strain is distinguished by a set of mutations that affect a significant functional region of the S-protein, which allows the new variant of the coronavirus to partially evade the action of antibodies in both people who have previously suffered COVID and those who have been vaccinated. And this feature makes the delta variant the most unfavorable of all the WHO-listed coronavirus strains that require special attention (it also includes British, Brazilian and South African variants) [14].
The risk of hospitalization in people with the delta variant of coronavirus is twice as high as in people with the alpha variant, but vaccines are effective against both varieties. Such data was published in the lancet journal by the national health service of Scotland when it analyzed the statistics of the incidence of coronavirus from April to June: during this period, the delta strain of coronavirus was spreading in India, but vaccination was already carried out [15-18].
It should be noted that the coronavirus changes over time and acquires new mutations that cause concern among scientists and doctors. In the UK, the dominant British strain (alpha variant) was replaced by the Indian strain (delta variant). Chris Robertson and colleagues from the national health service of Scotland studied how the incidence of coronavirus has changed. The scientists used patient information from the EAVE II platform, which contains medical data of 99% of the Scottish population. The analysis included the period from April 1 to June 6. According to researchers, by the end of May, about 70% of COVID cases were caused by the delta variant [19,20].
The researchers calculated the risk of hospitalization for patients with alpha and delta variants, adjusting for age, gender, concomitant diseases and time trend. It turned out that the risk of getting to the hospital with the delta variant is almost twice as high as with the alpha variant (HR=1.85). Simultaneously with the spread of the new variant, the population was vaccinated in Scotland: On April 1, 44.7% of people received the first dose of the vaccine, and 7.6% received the second. The vaccine developed by Pfizer showed 92% effectiveness against the alpha variant and 79% against the delta variant. The vaccine created by AstraZeneca was less effective: 73% against the alpha variant and 60% against the delta variant [21].
The researchers concluded that the Indian strain of coronavirus increases the risk of hospitalization by about two times, compared with the British one. At the same time, the vaccines are effective against both types of coronavirus. Recently, the US Centers for disease control and prevention reported on the incidence of coronavirus infection after vaccination. A total of 10,262 cases of infection were registered (per 101 million vaccinated), and 160 people died [22]. The second unpleasant feature of the Indian strain is the speed of its transmission from person to person. The virus has become more "tenacious": it attaches to cells faster, and a smaller dose of it is enough to infect cells. Inside the body, the delta variant is transmitted faster from cell to cell, reaching high concentrations in body tissues. At the same time, the incubation period was reduced. Epidemiologists from China report that several generations of the virus change in just 10 days, because it is able to be repeatedly transmitted from person to person during this period. Previously, the average incubation period for the transmission of one generation of the virus, that is, from one person to another, was 5-7 days [23].
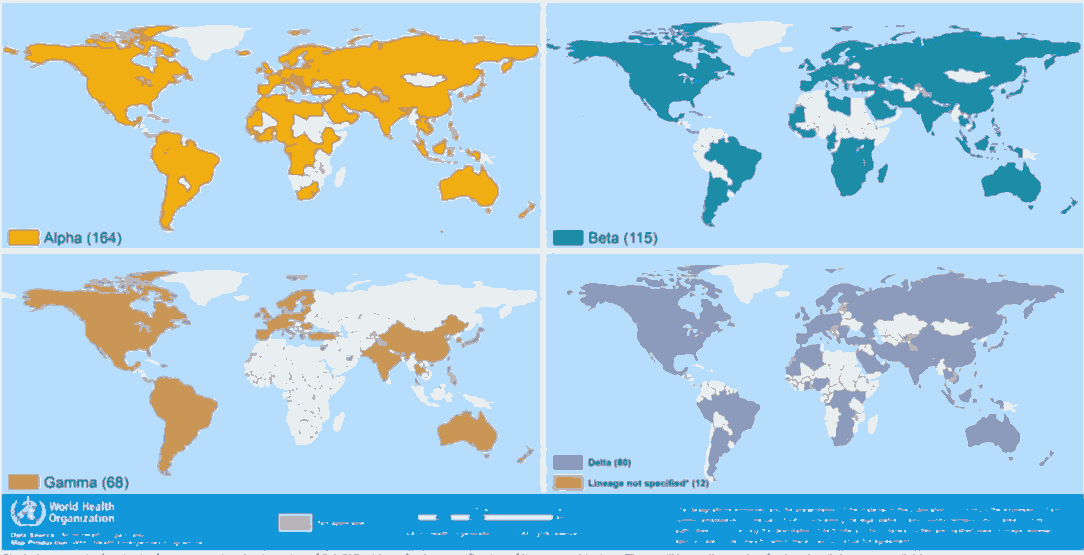
As of June 16, 13,397 cases of coronavirus infection were registered in Russia, and 5,782 infected people were registered in Moscow. In the next day, number of cases in the country increased by another 660 people, in Moscow-by 413. On Friday, 18.06.2021, a sharp jump was established: Coronavirus infection was confirmed in 17,262 Russians, more than half of them 9,056 residents of the capital. There was no such high indicator in Moscow for the entire time of the pandemic. Previously, the peak of the spread of SARS-COV-2 in the capital in one day was considered to be December 24, 2020, when 8,203 cases were detected [24]. Now those Western countries are coming out of isolation, Russia risks falling into a new vicious wave of the virus. And officials are beginning to recognize that the pandemic in the country will not end in the near future if the number of vaccinations does not sharply increase [25]. Next, we offer the spread of new strains of SARS-COV-2 in the world (Figure 1).
| WHO label | Pango lineage | GISAID clade | Next strain clade | Earliest documented samples | Date of designation |
|---|---|---|---|---|---|
| Variants of Concern (VOCs) | |||||
| Alpha | B.1.1.7 | GRY (formerly GR/501Y.Vl) | 201 (V ) | United Kingdom, Sep-2020 | 18-Dec-2020 |
| Beta | B.1.351 | GH/501Y.V2 | 20H (V2) | South Africa, May-2020 | 18-Dec-2020 |
| Gamma | P.1 | GR/501Y.V3 | 20J (V3) | Brazil, Nov-2020 | 11-Jan-21 |
| Delta | B.1.617.2 | G/478K.Vl | 21A | India, Oct-2020 | VOI: 4-Apr-2021VOC: 11-May-2021 |
| Variants of Interest (VOIs) | |||||
| Epsilon | B.1.427/ B.1.429 | GH/452R.Vl | 21C | United States of America, Mar-2020 | 05-Mar-21 |
| Zeta | P.2 | GR/484K.V2 | 20B/S.484K | Brazil, Apr-2020 | 17-Mar-21 |
| Eta | B.1.525 | G/484K.V3 | 21D | Multiple countries, Dec-2020 | 17-Mar-21 |
| Theta | P.3 | GR/1092K.Vl | 21E | Philippines, Jan-2021 | 24-Mar-21 |
| Lota | B.1.526 | GH/253G.V1 | 21F | United States of America, Nov-2020 | 24-Mar-21 |
| Kappa | B.1.617.1 | G/452R.V3 | 21B | India, Oct-2020 | 04-Apr-21 |
| Lambda | C.37 | GR/452Q.Vl | 20D | Peru, Aug-2020 | 14-Jun-21 |
Table 2. SARS-COV-2 weekly epidemiological update edition 44, published 15 June 2021.
Clinical Manifestations
Imperial college London studied more than a million people in England, while the alpha variant was dominant, and found a wide range of additional symptoms associated with SARS-COV-2. "Chills, loss of appetite, headache and muscle pain" were the most common in infected people, as were the classic symptoms. The new variant of the virus detected in India (delta variant) is 60% more contagious than the previous strains and in some cases leads to deafness, gangrene and amputation of limbs in patients. Children and animals get sick with this variant much more often and suffer the disease more severely than those who have picked up the British strain. Infected people experience severe pain in the joints and abdomen, nausea, vomiting and eventually lose their hearing, that is, they develop neurological complications. There are also many reports of blood clots in the blood vessels of the intestines and extremities [26].
Treatment
In general, the treatment of coronavirus infection is an experimental etiotropic drug (remdesevir), pathogenetic treatment (anticoagulant therapy, corticosteroids, NSAIDs, a drug based on monoclonal antibodies, convalescent plasma, with the development of complications-antibacterial therapy). In the United States, the FDA has approved for emergency use three drugs based on monoclonal antibodies against SARS-CoV-2 for the treatment of SARS-COV-2: bamlanivimab+etesevimab, casirivimab+imdevimab, and sotrovimab. Bamlanivimab+etesevimab, administered together for the treatment of mild and moderate coronavirus disease 2019 (SARS-COV-2) in adults and children (12 years and older with a body weight of at least 40 kg) with positive results of direct testing for the SARS-COV-2 virus and who have a high risk of developing severe SARS-COV-2 and/or hospitalization [2,18].
Vaccination
An effective way to prevent SARS-COV-2 and the development of severe forms is vaccination. An example of successful vaccination is Israel. The state has vaccinated 60% of the population, including 80% of people over 60 years old. Since 15.06.2021, vaccination of children from 12 years old has been started. 15.06.2021 the country canceled the mask mode. In the Republic of Kazakhstan, 4.16 million as of 16.06.2021, full vaccination of 1.53 million (8.2%). Thus, the dynamics of the increase in new cases of the disease is associated with the active spread of new variants of coronavirus after they occupy a dominant position, different in different countries and depends on the speed of introduction of anti-COVID measures and their sufficiency, the coverage of the population with vaccines and the level of collective immunity.
Conclusion
There is an increase in the Delta variant (Indian strain) of coronavirus in the world (in the UK, the delta variant is more than 90%, and at the end of May it was only 40%. In Moscow 89.3% of all new cases of coronavirus are associated with the Delta variant). As a rule, after 1.5-2 months after registration in the Russian Federation, a new strain comes to the Republic of Kazakhstan. The distinctive features are the shortening of the incubation period, high contagiousness and the rate of transmission of infection (one patient with the delta variant infects 5-6 people). Along with the classic symptoms of the disease, infected people experience severe pain in the joints and abdomen, nausea, vomiting, neurological complications may develop, and there is also evidence of the development of blood clots in the blood vessels of the intestines and extremities.
References
- https://www.aljazeera.com/news/2021/1/20/uk-new-covid-strain-reported-in-at-least-60-countries-who
- Collier D, Meng B, Ferreira I, et al. Impact of SARS-CoV-2 B.1.1.7 Spike variant on neutralisation potency of sera from individuals vaccinated with Pfizer vaccine BNT162b2. medRxiv 2021; pp: 11:24.
- Mahase E. Covid-19: what new variants are emerging and how are they being investigated? BMJ 2021; 372: 158.
- Volz E, Mishra S, Chand M, et al. Transmission of SARS-CoV-2 lineage B.1.1.7 in England: insights from linking epidemiological and genetic data. medRxiv 2021; pp: 1-37.
- West JAP, Barnes CO, Yang Z, et al. SARS-COV-2 lineage B. 1.526 emerging in the New York region detected by software utility created to query the spike mutational landscape. bioRxiv 2021; pp: 1-15.
- Tchesnokova V, Kulakesara H, Larson L, et al. Acquisition of the L452R mutation in the ACE2-binding interface of Spike protein triggers recent massive expansion of SARS-Cov-2 variants. bioRxiv. 2021; pp: 1-23.
- www.who.int/csr/don/31-december-2020-sarscov2--variants/en
- Alwan NA. Surveillance is underestimating the burden of the COVID-19 pandemic. Lancet 2020; 396(10252): e24.
- Hossain MK, Hassanzadeganroudsari M, Apostolopoulos V, et al. COVID-19 vaccines in the pipeline, are antibodies adequate vaccines MDPI 2021; 9(3): 241.
- Wang Z, Schmidt F, Weisblum Y, et al. mRNA vaccine-elicited antibodies to SARS-COV-2 and circulating variants. bioRxiv 2021; 592: 616–622.
- Ball P. The lightning-fast quest for COVID vaccines-and what it means for other diseases. Nature 2021; 589(7840): 16-18.
- Callaway E. The coronavirus is mutating-does it matter? Nature 2020; 585(7824): 174–177.
- Wise J. Covid-19: new coronavirus variant is identified in UK. BMJ 2020; 371: m4857
- Li D-D, Li Q-H. SARS-CoV-2: vaccines in the pandemic era. Mil Med Res 2021; 8(1): 1–15.
- Wibmer CK, Ayres F, Hermanus T, et al. SARS-CoV-2 501Y.V2 escapes neutralization by South African COVID-19 donor plasma. bioRxiv 2021; 27: 622–625.
- Wu K, Werner AP, Moliva JI, et al. mRNA-1273 vaccine induces neutralizing antibodies against spike mutants from global SARS-CoV-2 variants. bioRxiv 2021; 25: 1-12.
- Gupta R, Collier D, De Marco A, et al. SARS-CoV-2 B.1.1.7 escape from mRNA vaccine-elicited neutralizing antibodies Nature 2021; 593: 136–141.
- Xie X, Liu Y, Liu J, et al. Neutralization of spike 69/70 deletion, E484K, and N501Y SARS-CoV-2 by BNT162b2 vaccine-elicited sera. bioRxiv. 2021; 27(4): 620-621.
- https://www.bbc.com/news/world-africa-55975052
- https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html
- https://www.bloomberg.com/news/articles/2020-12-24/new-virus-strain-s-transmissibility-to-cause-more-deaths-study
- Nikpouraghdam M, Jalali Farahani A, Alishiri G, et al. Epidemiological characteristics of coronavirus disease 2019 (COVID-19) patients in IRAN: A single center study. J Clin Virol 2020; 127: 104378.
- Mizumoto K, Omori R, Nishiura H. Age specificity of cases and attack rate of novel Coronavirus Disease (COVID-19). medRxiv 2020; pp: 1-16.
- Choe YJ. Coronavirus disease-19: The first 7,755 cases in the Republic of Korea. medRxiv 2020; 11(2): 85-90.
- Jiehao C, Jin X, Daojiong L, et al. A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin Infect Dis 2020; 71: 1547-51.
- Kemelbekov K, Ospanova E, Baimakhanova B, et al. Epidemiological characteristics of new Coronavirus Diseases (COVID-19): Features of risk factors and clinical features of the child population. Electron J Gen Med. 2020; 17: em252.