Current Pediatric Research
International Journal of Pediatrics
Ascaris lumbricoides induced small bowel obstruction; experience from a tertiary care centre.
Raashid Hamid*
Department of Pediatrics, Sher-I-Kashmir Institute of Medical Science, Jammu and Kashmir, India
- Corresponding Author:
- Raashid Hamid
Department of Pediatrics,
Sher-I-Kashmir Institute of Medical Science,
Jammu and Kashmir,
India
E-mail: drraashidhamid@gmail.com
Received: 28 August, 2020, Manuscript No. AAJCP-24-18275; Editor assigned: 02 September, 2020, Pre QC No. AAJCP-24-18275 (PQ); Reviewed: 16 September, 2020, QC No. AAJCP-24-18275; Revised: 01 October, 2024, Manuscript No. AAJCP-24-18275(R); Published: 29 October, 2024, DOI: 10.35841/0971-9032.28.11.2384-2389.
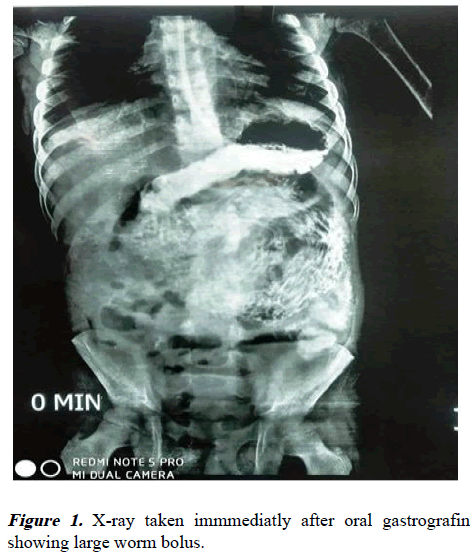
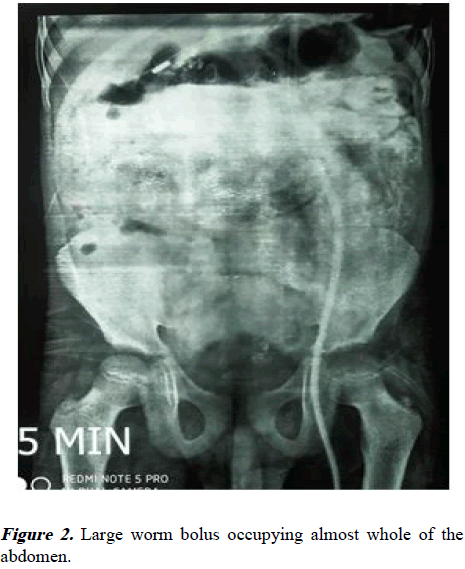
Introduction: Ascaris lumbricoides induced intestinal obstruction is a sequel of this parasitic infestation. It presents as colic, vomiting (bilious or non-bilious), abdominal distention and at times peritonitis. Management includes indoor admission, intravenous fluids, rectal enemas and serial clinical and radiological assessment for detecting any indication of surgery. We in our study we analysed the outcome of conservative management and use of oral administration of 76% gastrograffin. Methods: Clinical parameters of all these patients were recorded and kept under close monitoring of the clinical parameters. Patients were initially subjected to conservative treatment whereby patients were advised nil per oral, naso-gastric tube aspiration, intravenous fluid, rectal enemas and antibiotics as indicated. In some patients without signs of peritonitis and severe obstruction contrast agent gastrograffin was administered either per oral or via naso-gastric tube. Serial abdominal radiographs were taken. Surgical intervention was performed if worms were not expelled after 48-72 hr of conservative treatment or contrast gets held up after 24 to 36 hrs in small intestines or clinical deterioration. Data was analysed stastically. Results: A total of 240 patients were included in this study. The abdominal pain 156 (65%) was the most common symptom followed by distension in 168 (70%). Among patients, 65% were boys (n=156) and 35% girls (n=84). The clinical signs included abdominal distention in 168 (70%), tenderness in 28 (11%), rigidity 34 (14%), palpable worm masses in 115 (48%) and visible gut loops in 29 (23%). Most of the patients 204 (85%) responded to conservative management. Among 36 patients who needed surgery, 10 patients had received oral contrast. The pre-operative findings included-impacted worms in 14 cases, impacted worm mass with gangrene 6 cases, intussusceptions without gangrene 7 cases and gut volvulus with gangrene in 9 cases. The average hospital stay was 4.40 ± 2.25 days in cases managed conservatively, whereas about 10.35 ± 6.24 days in cases needing surgical intervention. There was no mortality in our series. Conclusion: Ascaris induced worm obstruction should be managed conservatively, surgery is indicated if conservative management does not result in clinical improvement. Addition of gastrograffin orally in some patients without complete obstruction significantly decreases the hospital stay and reduces the time period between admission to expulsion of the worms.
Keywords
Ascaris lumbricoides, Conservative management, Obstruction, Gastrografin.
Introduction
Ascaris lumbricoides (A. lumbricoides) is the most common tropical intestinal helminth parasite and it is estimated that the infested population is 0.8-1.2 billion worldwide. Ascariasis can occurs in all ages, but it is most common in children between 2 to 10 years of age and prevalence decreases above the age of 15 years. The massive infestation in children can result in serious complications, which include obstruction of the small intestine, appendiceal lumen, bile duct and pancreatic duct. Intestinal volvulus, intussusceptions, peritonitis due to perforation of a viscus is also common. Intestinal obstruction has been estimated to occur in 2 per 1000 ascarisis-infested children per year. Conservative treatment for partial intestinal obstruction due to round worm is practised worldwide. In this study, we present our experience of conservative treatment for intestinal obstruction due to ascariasis. We evaluated clinical history, examination, investigations and management, either conservative or operative. Various surgical procedures with preoperative findings were noted.
Materials and Methods
All the patients with suspected round worm intestinal obstruction who were admitted in Paediatric Surgery Department of Sheri-Kashmir Institute of Medical Sciences, India from 2010-2019 were included in study. Patients who presented with sign and symptom of peritonitis or perforation were excluded from our study. A total of 240 patients of intestinal ascariasis were admitted during this period. All these patients were kept under close monitoring of the parameters including heart rate, abdominal girth, nasogastric aspirate, hydration status, serum electrolytes, total and differential blood counts and radiographic findings. All patients were initially subjected to conservative treatment whereby patients were advised nil per oral, naso-gastric tube aspiration, intravenous fluid, rectal enemas and antibiotics as indicated.
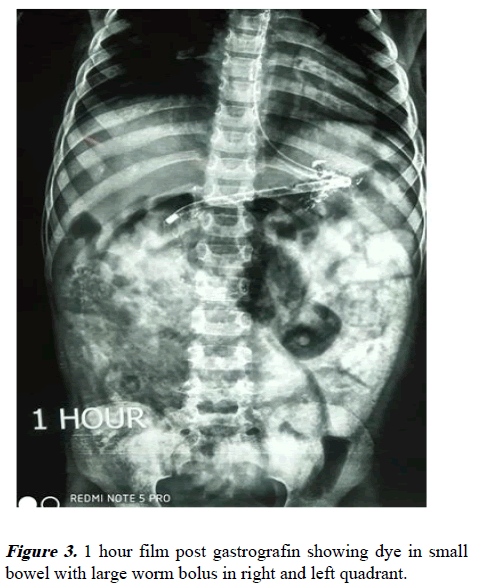
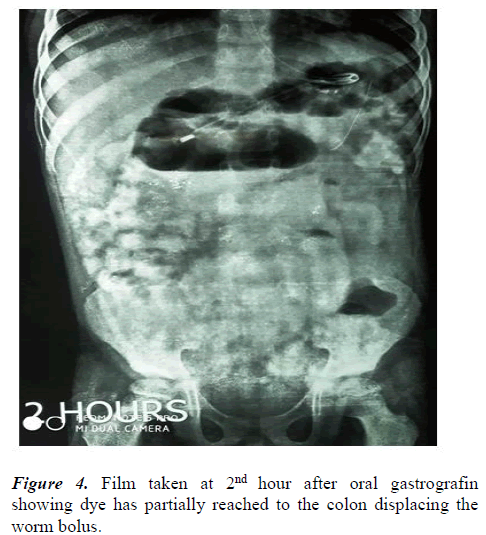
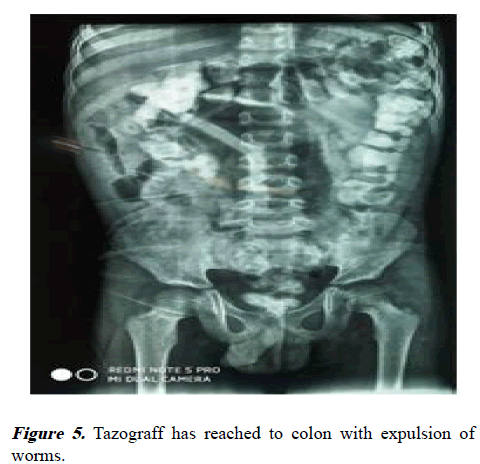
In some patients without obstruction contrast agent diatrizoate meglumine 76% (tazograff) was administered either per oral or via naso-gastric tube. The patients were monitored with serial assessment of vital parameters and abdominal girth measurement. Serial abdominal radiographs were taken at 0, 6, 24 and 48 h. Clinical improvement was defined as a decrease in abdominal pain and distension, decrease in abdominal girth and associated passage of flatus or stool. In children who received diatrizoate meglumine, the clinical improvement was defined when the contrast reached to the colon within 24 to 36 hours along with passage of flatus or stool. The treatment included appropriate intravenous fluid, nasogastric aspiration, antispasmodic drugs and antibiotics followed by rectal enemas. The patients were considered for surgical intervention, if worms were not expelled after 48-72 hr of conservative treatment or contrast gets held up after 24 to 36 hrs in small intestines or clinical deterioration. Clinical deterioration included increasing abdominal distension, guarding and rebound tenderness bleeding per rectum, persistence of worm mass at the same site or fixity of mass. Out of 240 patients only 32 (13.6%) patient required surgical exploration. We used right transverse incision in all cases. In those cases were resection and anastomaosis was needed for the gut gangrene, single layer interrupted anastomosis was performed between two healthy edges of the small gut. The post-operative orals sips were started at 48-72 hours. In instances when there were large boluses of worms not amenable to kneading to either colon or stomach, an enterotomy was made for retrieval of the worms. The enterotomy was made longitudinally and closed transversally. The patients with enterotomy were given oral sips at 48 hours. The operative notes included preoperative findings as: Site of worm mass/masses, condition of gut and mesentry lymph nodes. All patients were advised to attend follow-up clinics.
Results
A total of 240 patients were studied in the range 12 months-12.6 (average-7.35 ± 2.25 years) with commonest age of presentation 3-7 years (60%). The most of the patients presented with abdominal pain 156 (65%) and distension 168 (70%). About 108 (45%) patients passed worm in vomitus and 152 (63.6%) patients passed worms per rectally (Table 2). Among patients, 65% were boys (n=156) and 35% girls (n=84). The average duration of illness (in days) at the time of presentation was 1.84 ± 1.20 days. A total of 168 patients (70%) were from rural areas and 30 patients (24%) belonged to urban areas. Only 12 patients (5%) belonged to high socioeconomic class, 168 patients (70%) belonged to low socioeconomic class. The colicky peri-umbilical abdominal pain was the most common symptom present in 144 (60%) of patients while as vomiting was the second leading symptom. 25% patients had history of worms in vomitus while 40% (n=108) children presented with constipation. In 23% (n=55) patients there was history of passage of worms in stool after anti-helminthic treatment in recent past.
| Symptom | Frequency | Percentage |
|---|---|---|
| Pain abdomen | 156 | 65 |
| Vomiting | 108 | 45 |
| Distension of abdomen | 168 | 70 |
| Constipation | 108 | 48 |
| Fever | 8 | 10 |
| Dehydration | 67 | 28 |
Table 1. Clinical symptoms at the time of presentation in patients.
Of all twenty patients (8%) had past history of worm infestation. Sixty-seven (28%) patients presented with dehydration. Other signs included fever in 24 (10%) patients, pallor in 66 (27%) patients and emaciation in 15 (6%) patients. The clinical signs included abdominal distention in 168 (70%), tenderness in 28 (11%), rigidity 34 (14%), palpable worm masses in 115 (48%) and visible gut loops in 29 (23%). Some patients had more than one clinical finding (Table 2). X-ray abdomen and ultrasonography features revealed maximum quadrant palpable worm mass was seen in umbilical quadrant. The whirlpool sign was present in 84 (35%) of cases. Other signs on radiograph and ultrasonography included distended gut loops, multiple air fluid levels, worm bolus, inter loop fluid, fluid in pelvis (Table 3). Ultrasonographic finding were positive in 192 (80%). Investigations included haemogram and liver function. Hemoglobi<10.0 gm% was seen in 80 (33%) of patients. Eosinophilia was seen in 40 (17%) patients. 204 (85%) were managed conservatively and 36 (15%) underwent surgery. Among 36 patients who needed surgery, 10 patients had received oral contrast. The pre-operative findings included-impacted worms in 14 cases, impacted worm mass with gangrene 6 cases, intussusceptions without gangrene 7 cases and gut volvulus with gangrene in 9 cases. Eleven cases needed enterotomy and in 7 cases worms could be milked to colon. Thirteen patients underwent resection anastomosis of ilium. The average hospital stay was 4.40 ± 2.25 days in cases managed conservatively, whereas about 10.35 ± 6.24 days in cases needing surgical intervention. There was no mortality in our series.
| Clinical signs | Frequency | Percentage |
|---|---|---|
| Distension of abdomen | 168 | 70 |
| Abdominal tenderness | 28 | 11.8 |
| Rigidity and guarding | 24 | 10 |
| Palpable worm masses | 11 | 48 |
| Visible gut loops | 55 | 23 |
| Visible worm masses | 33 | 14 |
| Dehydration | 67 | 28 |
Table 2. Clinical signs observed in patients.
| Radiographic features | Frequency | Percentage |
|---|---|---|
| Distended bowel loops | 192 | 80 |
| Worm bolus | 168 | 70 |
| Multiple air-fluid level | 115 | 48 |
| Inter-loop fluid | 26 | 11 |
| Free fluid in pelvis | 14 | 6 |
Table 3. Abdominal x-ray and USG findings of worm obstruction.
| Pre-operative findings | Frequency | Percentage |
|---|---|---|
| Impacted worm masses | 14 | 5.83 |
| Impacted worm masses with gangrene | 6 | 2.5 |
| Intussusception without gangrene | 7 | 2.91 |
| Gut volvulus with gangrene | 9 | 3.75 |
Table 4. Pre-operative findings in patients who underwent surgery.
| Surgical procedure | Frequency | Percentage |
|---|---|---|
| Enter-otomy | 11 | 4.5 |
| Kneading of worms | 7 | 2.91 |
| Reduction of intussusption | 5 | 2.08 |
| Resection anastomosis | 11 | 4.58 |
Table 5. Operative procedure performed.
Discussion
The intestinal ascariasis is most common parasite infestation of human beings and it affects one fourth of world population. It can lead to symptomatic illness and death. Ascarisis is highly endemic in this part of India. The most infested persons are asymptomatic with clinical disease of restricted to subjects with heavy worm-load. The majority of patients present in the first decade of life. The rural areas have more prevalence of round infestation due to low socioeconomic status, poor hygiene and cultural factors. The symptomatic patients present with dehydration, pallor and emaciation. Some patients had history of expulsion of worms per rectum or mouth which help in making a right diagnosis. As demonstrated in our study various symptoms include abdominal pain, vomiting, constipation, loose motions, ascaris in vomitus and passage of worms in stool.
In our series abdominal distension, tenderness, guarding and palpable worm masses were observed on abdominal examination. The distribution of pain with reference to quadrant of abdomen shows periumbilical quadrant being commonest. As the jejunum and proximal ileum are the usual habitat of roundworm around the peri-umblical area, which results in periumbilical pain area. The worm masses are palpable around umbilical quadrant as worms usually conglomerate in the distal jejunum. Worm bolus has a characteristic frequent directional change of position and breaking into small boluses. Disentangled worm bolus pass ileocecal valve under conservative treatment. In our series ascaridial lump disappeared from right iliac fossa within 48 to 72 h with conservative management. The change in position of palpable worm masses should be one of the criteria for assessing efficacy of conservative treatment. The plain radiography and ultrasonography of the abdomen may reveal evidence of subacute or acute intestinal obstruction or features of peritonitis. A characteristic “cigarette ash” appearance of worm mass is usual appearance on x-ray. The abdominal x-ray shows air fluid levels and multiple linear images of Ascaris lumbricoides in the dilated intestinal loops and whirlpool sign was suggestive in 35% cases in the present study which is slightly less than other reported series. Ultrasonography diagnosed 80% of cases in present study and is comparable to other reported series.
The serial radiological assessment is important to assess progress of conservative treatment. Our conservative management for symptomatic intestinal ascariasis is similar to those reported by Surendran and Paulose, Dayalan and Ramakrishnan, Waller and Othersen. With regards to conservative management, our results are similar with numerous studies reported in the literature who managed the majority of their cases conservatively.
The mechanical obstruction of gut by worms is the commonest mode of intestinal obstruction. Other causes of ascaridial small gut obstruction include volvulus or intussusception. Intussusception can be jejuno-ileal, ileo-ileal or jejuno-jejunal. The worm inside vermiform appendix may incite appendicitis. Surgical intervention must always be weighed against the stigmata of morbidity and mortality of surgery. The criteria taken into account for deciding surgical intervention simulate those observed by Dayalan and Ramakrishnan and Louw. Based on the above criteria, 12 (22%) of 360 cases were subjected to operative intervention. The pre-operative findings can be decisive in selecting cases for surgical procedure to be done. The factors for kneading or the enterotomy for worms are site of worm bolus, number of worm boluses, length of worm bolus, pressure on intestinal wall by worm bolus and transerosal visibility of worms. Enterotomy for removal of worms should be performed when there is trans serosal visibility, otherwise kneading of worms to the large gut is sufficient. Enlarged mesenteric nodes can be seen with size and number depending on hyper-infestation with worms and the presence of any secondary infection. Only 1% of 79 cases had mortality compared with the observations of Ochoa who had mortality of 8.27% of cases in operative series of patients. Mukhopadhyay et al. had mortality of 2.39% in his operative series of patients.
Conservative management for partial worm obstruction is advocated in many studies and can be managed with intravenous fluid administration, nasogastric suction and instillation of oral piperazine salt, normal saline enema and hypertonic saline enemas. Few studies advocated use of gastrografin. For evacuation of worms with variable results. Use of gastrografin resulted in faster relief of signs and symptoms of round worm-induced small bowel obstruction, early passage of worms or flatus and return to oral feeds. Mukhopadhyaya et al., used anthelminthic drug along with normal saline enema and reported 50% success to conservative treatment in their series. All these studies advocated conservative management in cases of partial worm obstruction only, but in present study we have used conservative treatment in patients with complete intestinal obstruction without sign and symptoms of perforation and peritonitis due to round worms.
The results of our study are similar with Mukhopadhyay et al. who did not have any mortality in the conservative series. Early detection of disease, well acquaintance with disease, avoidance of delay for those requiring surgical intervention, appropriate antibiotic cover and serial radiological assessment helped to reduce morbidity and mortality.
Conclusion
Intestinal asicarisis is still endemic in children belonging to rural areas and low socio-economic strata of the society. Colicky periumbilical pain and distension of abdomen are common initial presenting symptoms. Serial plain radiograph of abdomen and pelvis are useful for early diagnosis and management. The conservative management is successful in most of the cases. Surgical intervention is required for complicated intestinal ascariasis.
References
- Drake LJ, Bundy DA. Multiple helminth infections in children: Impact and control. Parasitology 2001; 122: S73-S81.
[Crossref] [Google Scholar] [PubMed]
- Villamizar E, Mendez M, Bonilla E, et al. Ascaris lumbricoides infestation as a cause of intestinal obstruction in children: Experience with 87 cases. J Pediatr Surg 1996; 31: 201-205.
[Crossref] [Google Scholar] [PubMed]
- Akgun Y. Intestinal obstruction caused by Ascaris lumbricoides. Dis Colon Rectum 1996; 39: 1159-1163.
[Crossref] [Google Scholar] [PubMed]
- Khuroo MS. Ascariasis. Gastroenterol Clin North Am 1996; 25: 553-577.
[Crossref] [Google Scholar] [PubMed]
- Rahman H, Pandey S, Mishra PC, et al. Surgical manifestations of ascariasis in childhood. J Indian Med Assoc 1992; 90: 37-39.
[Google Scholar] [PubMed]
- Surendran N, Paulose MO. Intestinal complications of round worms in children. J Pediatr Surg 1988; 23: 931-935.
[Crossref] [Google Scholar] [PubMed]
- Dayalan N, Ramakrishnan MS. The pattern of intestinal obstruction with special preference to ascariasis. Indian Pediatr. 1976; 13: 47-49.
[Google Scholar] [PubMed]
- Waller CE, Othersen Jr HB. Ascariasis: Surgical complications in children. Am J Surg 1970; 120: 50-54.
[Crossref] [Google Scholar] [PubMed]
- Louw JH. Abdominal complications of Ascaris lumbricoides infestation in children.
[Crossref] [Google Scholar] [PubMed]
- Ochoa B. Surgical complications of ascariasis. World J Surg 1991; 15: 222-227.
[Crossref] [Google Scholar] [PubMed]