Current Pediatric Research
International Journal of Pediatrics
Early detection of neonatal sepsis using platelet indices as diagnostic markers.
S Manazir Ali*, Saba Samreen, Uzma Firdaus, S H Arif
Department of Pediatrics, Aligarh Muslim University, Uttar Pradesh, India
- Corresponding Author:
- S Manazir Ali
Department of Pediatrics,
Aligarh Muslim University,
Uttar Pradesh,
India
E-mail: manazir1958@yahoo.com
Received: 13 July, 2020, Manuscript No. AAJCP-24-15399; Editor assigned: 16 July, 2020, Pre QC No. AAJCP-24-15399 (PQ); Reviewed: 30 July, 2020, QC No. AAJCP-24-15399; Revised: 01 October, 2024, Manuscript No. AAJCP-24-15399 (R); Published: 29 October, 2024, DOI: 10.35841/0971-9032.28.10.2368-2372.
Introduction: Neonatal septicemia is a major reason which may lead to an increase in mortality so if diagnosis is made in time and proper management done, it may help in providing adequate antibiotic coverage and preventing the morbidity and mortality of babies. Aim and objective: The primary objective of this study was to find the prevalence of thrombocytopenia, Mean Platelet Volume (MPV), Platelet Distribution Width (PDW) and plateletcrit among the cases of culture positive and culture negative sepsis. Materials and methods: A hospital based observational study was conducted during the period from October 2017-August 2019 in NICU. A total of 208 neonates were taken and were divided into cases having culture proven sepsis (n=57), probable sepsis (n=47) who met the inclusion criteria along with normal healthy controls (n=104) which were comparable to the study group. All of neonates were subjected to detailed history including maternal history and signs and symptoms of sepsis. Blood investigation for complete blood count including platelet indices and blood culture were sent. Neonates born <34 weeks and those born with congenital anomalies were excluded from the study. Result: Among the cases 57 (54.8%) neonates had culture proven sepsis. Thrombocytopenia was seen in 76.9% of cases. Among cases 34 (32.7%) neonates expired. Platelet counts were low in culture proven cases (p<0.01) with similarly significant results in MPV (p<0.01), PDW (p<0.01) and plateletcrit (p<0.01). Most common organism isolated in sepsis was Klebsiella pneumonia (35%). Conclusion: Thrombocytopenia is a common complication associated with neonatal sepsis having a higher mortality rate. MPV is also a reliable markers along with PCT. PDW can also be added as an additional tools to detect early onset septicemia.
Keywords
Neonatal septicemia, Thrombocytopenia, Blood culture, Klebsiella pneumoniae.
Abbreviations
MPV: Mean Platelet Volume; PDW: Platelet Distribution Width; NICU: Neonatal Intensive Care Unit; CONS: Coagulase Negative Staphylococci; J.N.M.C.H: Jawaharlal Nehru Medical College; A.M.U: Aligarh Muslim University
Introduction
Neonatal sepsis is characterized by signs and symptoms of infections which may be associated with bacteremia presenting mainly during the first month of life and may lead to an increase in deaths of new born. The exact magnitude of neonatal sepsis in India is not known but as per national neonatal prenatal database (2002-2003); 30 cases per 1000 live births had neonatal sepsis which was approximately 19% of the neonatal mortality which occurred in India. Neonatal septicemia is divided into two types:
Early Onset neonatal Sepsis (EOS): It occurs within 72 hours of birth due to organisms present in the surrounding delivery area or present in the female genital tract.
Late Onset neonatal Sepsis (LOS): It occurs after 72 hours of birth mainly caused by microorganisms which are present in surrounding external environment.
Diagnosis of sepsis in neonates is based on the gold standard that is the blood culture but the results are available after a period of 48-72 hours which are frequently falsely negative. Blood culture positivity occurs in 25%-70% cases. So, initiation of antibiotics in suspected neonatal sepsis may lead to unnecessary increase in the antibiotic consumption which subsequently may give rise to high incidence of resistance to them [1].
MPV measures the size of the platelet present in blood. Neonatal sepsis is frequently associated with elevation in MPV and PDW. In neonates the sensitivity of MPV in diagnosing sepsis is 54% and specificity is 82%. Guclu et al. in his study confirmed, there was a significant difference in the values of PDW and MPV among the sepsis cases and control group. Thrombocytopenia is a complication that commonly is present in critically ill patients.
Riedler et al. reported thrombocytopenia in 80% of sepsis cases were caused by gram negative organisms and 65% by gram positive organisms. In neonatal sepsis damage to the endothelial lining occurs which leads to activation of reticuloendothelial system causing the removal of the platelets, due to this the platelet consumption is more than the platelet production ultimately leading to thrombocytopenia [2].
There have been many studies suggesting different parameters for early diagnosis of sepsis but not a definite parameter has been found. An observational study utilizing platelet indices as early markers to diagnose neonatal septicemia in the patients of culture positive and culture negative sepsis has been conducted.
Aim
To find the prevalence of thrombocytopenia, platelet distribution width, mean platelet volume and plateletcrit in cases of culture positive and culture negative neonatal sepsis.
Objectives
Primary: To assess the efficacy of platelet indices alone and in combination in newborns having sepsis.
Secondary: To find out etiological agents causing neonatal sepsis and to find out the mortality rate of neonatal septicemia.
Materials and Methods
This study was a hospital based observational study conducted in the neonatal intensive care unit, department of pediatrics in collaboration with the department of pathology JNMCH AMU, Aligarh from October 2017-August 2019. Two hundred and eight babies having gestational age 36-38 weeks with birth weight >2500 g (cases=104; controls=104) were taken up for study. The babies who were up to seven days of age and presented with the signs or symptoms of sepsis were taken as the study population. All neonates with congenital malformations, who received antibiotic prior to blood sampling and less than 34 weeks, were excluded from study. The ethical clearance was obtained from the institutional ethics committee, JMNCH, Faculty of Medicine, AMU Aligarh [3].
Brief procedure
A proper consent was taken from the parents of neonates followed by a complete history along with signs of sepsis were properly evaluated. Blood was withdrawn and was divided for measurement of CBC, platelet count, PDW and MPV using the Nihon Kohdencelltac analyzer [4]. Blood culture and sensitivity was done by taking 1 ml-2 ml of blood in Mc Cartney’s blood culture bottle taking all aseptic precautions. Culture was incubated at 37°C, initial reporting done at 24 hours and final reports were seen after 5 days. All cases were further divided into two following groups:
Study group: Approximately 104 cases of sepsis were taken and divided into: a) Group A-Proven sepsis (Septicemia) characterized by neonates with clinical sepsis along with laboratory evidence and having a positive blood culture test, b) Group B-Probable sepsis characterized by neonates with clinical sepsis along with laboratory evidence as per IMNCI/WHO criteria but having a negative blood culture test, c) Group C-Control/No sepsis 104 neonates were taken having no clinical sepsis and normal laboratory parameters. Reference range for the parameters taken:
Platelet count: Thrombocytopenia when platelet count less than 150 × 103/μL.
• Severe thrombocytopenia less than 50 × 103/μL
• Moderate thrombocytopenia 50-100 × 103/μL
• Mild thrombocytopenia 100-150 × 103/μL
Mean platelet volume: Normal value of MPV-8.21 ± 0.658.
Platelet distribution width: Normal value if PDW 17.03 ± 0.078.
Statistical analysis: The analysis was done using the SPSS software version 25.
Results
208 new born were a part of this study. 104 were controls and 104 were sepsis patients among which there were 41 males and 63 females. Gender, mode of delivery and birth weight were compared between septic patients and the control group (Table 1) [5].
| Parameters | Grp-A (N=57) | Grp-B (N=47) | Grp-C (N=104) | P value |
|---|---|---|---|---|
| Gender (No. %) | ||||
| Male | 12 (21.1%) | 29 (61.7%) | 53 (50.9%) | 0.19 |
| Female | 29 (50.8%) | 34 (72.3%) | 47 (45.2%) | |
| Mode of delivery | ND=20 (48.8%) | ND=35 (55.6%) | ND=57 | 0.13 |
| LSCS=21 (51.2%) | LSCS=28 (44.4%) | LSCS=43 | 0.52 | |
| Birth weight | 2.76 ± 0.33 | 2.72 ± 0.28 | 2.74 ± 0.24 | 0.56 |
Table 1. Demographic comparison between cases and controls.
The most common symptom seen in the sepsis patient was that of respiratory distress (82.7%) in form of tachypnea, grunting, retractions, increased work of breathing followed by poor suck (78%), jaundice (72.1%) and lethargy (67.3%) (Table 2) [6].
| Criteria for sepsis | Number | Percentage |
|---|---|---|
| Respiratory distress | 86 | 82.70% |
| Poor suckling | 81 | 78% |
| Lethargy | 70 | 67.30% |
| Jaundice | 75 | 72.10% |
| Abdominal distension | 25 | 24.10% |
| Seizures | 27 | 25.90% |
| Apnoea | 10 | 9.60% |
| Vomiting | 40 | 38.50% |
| Bleeding | 44 | 42.30% |
| Hypothermia | 30 | 28.80% |
| Diarrhoea | 8 | 7.69% |
| Hypoglycaemia | 34 | 32.60% |
| Hyperthermia | 15 | 14.42% |
Table 2. Signs and symptoms indicating sepsis in the cases (N=104).
Blood culture was positive in 57 (54.8%) of the sepsis patients and 47 (45.2%) had culture negative sepsis. In this study Klebsiella pneumoniae (35%) was most commonly isolated organism and was followed by Pseudomonas (19.3%).
In the sepsis patients thrombocytopenia was observed in 76.9% of them and in the control group thrombocytopenia was observed in 9% of patients (p<0.01). Out of the 104 sepsis patients severe thrombocytopenia was seen in 26 (25%) of them. In the control group the patients with low platelet count had mild thrombocytopenia. In group A the average platelet count was lower as compared to group B and also significantly lower than the group C. The average MPV in group A was 11.35 ± 1.9 fL and in group B was 10.28 ± 2.45 fL which was significantly higher than the group C (Table 3) [7].
| Laboratory parameters | Grp A (N=57) x ± SD | Grp B (N=47) x ± SD | Grp C (N=100) x ± SD | P Value |
|---|---|---|---|---|
| Platelets (× 103/µL) | 82.5 ± 59 | 121.12 ± 57.5 | 262.7 ± 100.2 | <0.001 |
| MPV(fL) | 11.02 ± 2.37 | 10.04 ± 2.1 | 7.503 ± 0.7 | <0.001 |
| PDW | 18.1 ± 1.85 | 17.3 ± 1.75 | 16.57 ± 1.19 | <0.001 |
| PCT | 0.077 ± 0.046 | 0.09 ± 0.04 | 0.13 ± 0.04 | <0.001 |
Table 3. Comparison between the groups based on blood parameters.
On sub group analysis between group A and group B, significant p values were obtained among the laboratory parameters except in plateletcrit where p value was 0.4 (not significant).
Thrombocytopenia showed a 94.7% sensitivity and 47% specificity in the sepsis patients and when combined with MPV had a sensitivity of 79.6% and a specificity of 81% (Table 4).
| Parameters | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|---|---|---|---|---|
| Thrombocytopenia | 94.70% | 78.90% | 67.50% | 87.50% | 72.10% |
| MPV | 77.20% | 63.20% | 66.70% | 65.80% | 66.30% |
| PDW | 63.20% | 48% | 59% | 46.20% | 55.70% |
Table 4. Diagnostic validity of laboratory parameters in neonatal septicaemia.
There is a statistically significant negative correlation is seen of platelet count with MPV and PDW (Table 5).
| Laboratory parameters | Platelet count | |
|---|---|---|
| R value | p value | |
| MPV | -0.534 | p<0.001 |
| PDW | -0.489 | p<0.003 |
Table 5. Correlation of platelet count with the other laboratory parameters.
We also found that mortality rate in the thrombocytopenic patients was 28. 52 new born were discharged (Table 6) [8].
| Platelet count | Expired | Discharged |
|---|---|---|
| Thrombocytopenia (<150000/µL) | 28 | 52 |
| Platelet (>150000/µL) | 6 | 18 |
Table 6. Mortality rates associated with thrombocytopenia.
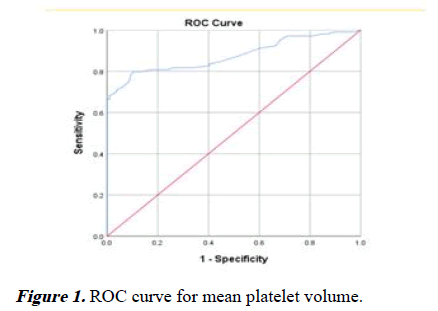
ROC curve was calculated for the detection of the cut off points of the various parameters. The cut-off point of MPV is 10.75 fL with a 77% and 65% sensitivity and specificity respectively (Figure 1).
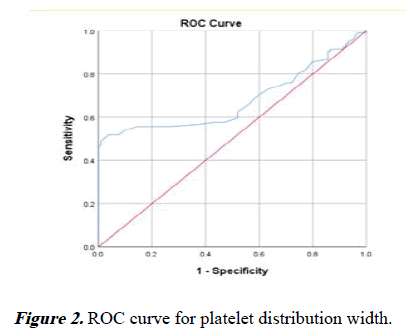
PDW showed a cut-off point of 17.25 with a sensitivity of 68.4% and 48.9% specificity (Figure 2).
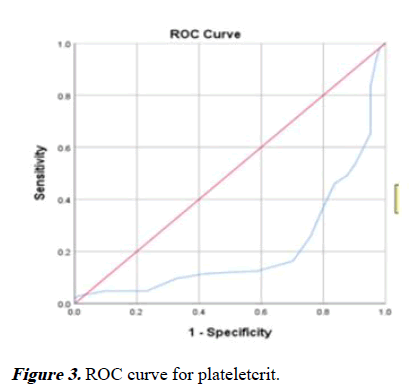
Plateletcrit showed a cut-off point of 0.085 with a sensitivity of 47.4% and 30.3% specificity (Figure 3).
Discussion
Septicaemia is one of the main causes of neonatal mortality. Hence there is a requirement for an early diagnosis of neonatal sepsis so as to start treatment of the neonate in cases of probable sepsis in order to decrease the occurrence of severe complications. This study aimed to find out the early predictors in form of platelet count, MPV, PDW, plateletcrit for the early diagnosis of neonatal septicaemia [9].
In this study, presenting clinical features of neonatal sepsis revealed that respiratory distress (82%), poor suck (78%) were the common clinical features. Similar result was seen in another study done by Mustafa which also showed a similar clinical presentation. This study showed a significant decrease in the platelet count along with an increase in the MPV and PDW in the cases of neonatal sepsis as compared to the control group. Similar results have been seen in other studies [10].
Blood culture was positive in 57 (54.8%) of the sepsis patients and 47 (45.2%) had culture negative sepsis, but in other studies done by Hisamuddin et al. found that culture proven sepsis was only 30%. Similar high positive blood culture was reported by Heena et al. having a positivity rate of 63%. The number of culture positive results depends on any previous antibiotic treatment, the time when sample is withdrawn and also the extent of bacteraemia in the neonate. In this study Klebsiella pneumoniae (35%) was most commonly isolated organism and was followed by Pseudomonas (19.3%), similar results were also seen in other studies. In our study thrombocytopenia was seen in 76.9% cases of sepsis. Study done by Guida et al. observed thrombocytopenia in 54% of the sepsis cases. Other studies have shown that thrombocytopenia is more severe if caused by gram negative sepsis as compared to infection caused by gram positive sepsis. In this study we observed that in sepsis cases the MPV was higher as compared to the controls. Similarly, Aydin et al. also reported that MPV was high in neonatal sepsis compared to healthy new born. These findings differed with a study done by Aksoy et al. in which it was observed that in between the septic and control infants MPV did not show significant difference. In this study a statistically negative correlation of MPV is showed with platelet count. Aydin et al. study also had similar correlation results. In this study the cut off of MPV is 10.75 fL to detect sepsis having 77% sensitivity and a 65% specificity. Septic patients have a higher PDW than controls. Similar results in PDW were also seen in the study by Narayan. Guclu showed statistically that the patient with a PDW higher than 18% had higher risk of death.
Conclusion
It is stated that neonatal infection is a major reason of neonatal thrombocytopenia. Present study concludes that platelet count was significantly decreased and PDW and MPV were increased in the septic neonates. The use of platelet volume indices as a definite parameter to detect infections is still not much in use as proper data regarding cut off values is lacking. Therefore, there is a need to standardize the measurement of platelet volume indices in order to get better results in detection of neonatal septicaemia.
Limitations
The new born population size taken was small. Withdrawal of blood in neonates for investigations is difficult and it may itself lead to contamination and sepsis. Presence of cell fragments and clumps may affect the proper assessment of indices.
Recommendation
By this study we can state that when platelet count and MPV is used in combination, it has a higher sensitivity and specificity compared to its individual use in diagnosis of neonatal septicaemia.
Acknowledgement
The authors would like to acknowledge the personnel (doctors, nurses, attendants and technician) staff working in the NICU and those personnel employed in clinical pathology department in J.N.M.C.H.
Conflict of Interest
No conflict of interest present between the authors.
References
- Mazhar A, Rehman A, Sheikh MA, et al. Neonates-a neglected paediatric age group. J Pak Med Assoc 2011; 61: 22204232.
[Google Scholar] [PubMed]
- Chandna A, Rao MN, Srinivas M, et al. Rapid diagnostic tests in neonatal septicemia. Indian J Pediatr 1988; 55: 947-953.
[Crossref] [Google Scholar] [PubMed]
- Guclu E, Durmaz Y, Karabay O. Effect of severe sepsis on platelet count and their indices. Afr Health Sci 2013; 13: 333-338.
[Crossref] [Google Scholar] [PubMed]
- Aydın B, Dilli D, Zenciroglu A, et al. Mean platelet volume and uric acid levels in neonatal sepsis. Indian J Pediatr 2014; 81: 1342-1346.
[Crossref] [Google Scholar] [PubMed]
- Riedler GF, Straub PW, Frick PG. Thrombocytopenia in septicemia. A clinical study for the evaluation of its incidence and diagnostic value. Helv Med Acta 1971; 36: 23-38.
[Google Scholar] [PubMed]
- Ree IM, Fustolo-Gunnink SF, Bekker V, et al. Thrombocytopenia in neonatal sepsis: Incidence, severity and risk factors. PloS One 2017; 12: e0185581.
[Crossref] [Google Scholar] [PubMed]
- Kim KY, Kim KE, Kim KH. Mean platelet volume in the normal state and in various clinical disorders. Yonsei Med J 1986; 27: 219-226.
[Crossref] [Google Scholar] [PubMed]
- Reyes JL, Robles MA, Ramirez RP, et al. Etiology and antimicrobial resistance patterns in early and late neonatal sepsis in a neonatal intensive care unit. Arch Argent Pediatr 2015; 113: 317-323.
[Crossref] [Google Scholar] [PubMed]
- Mustafa S, Farooqui S, Waheed S, et al. Evaluation of C-reactive protein as early indicator of blood culture positivity in neonates. Pak J Med Sci 2005; 21: 69-73.
- Hisamuddin E, Hisam A, Wahid S, et al. Validity of C-Reactive Protein (CRP) for diagnosis of neonatal sepsis. Pak J Med Sci 2015; 31: 527.
[Crossref] [Google Scholar] [PubMed]