Current Pediatric Research
International Journal of Pediatrics
Congenital icthiosiform erythroderma with vitamin D deficiency rickets in a 12 year old Indian boy.
Goutham AS*, Prasoon Bhatacharjee
Department of Pediatrics, Ananta Institute of Medical Sciences, Rajasthan University of Health Sciences, Rajasthan, India
- Corresponding Author:
- Goutham AS
Department of Pediatrics
Ananta Institute of Medical Sciences
Rajasthan University of Health Sciences
Rajasthan
India
Tel: 9469451875
E-mail: hamidraashid@gmail.com
Accepted date: 29th October, 2021
An ichthyosis is a heterogeneous group of skin disease characterized by generalized scaling. Congenital Ichthyosiform erythroderma is an autosomal recessive disorder with a mutation in the TGM 1 gene encodes the transglutaminase I protein was found. The scales reflect changes in epidermal differentiation. Congenital ichthyosiform erythroderma is the one of the rarest form of ichthyosis where the infant is usually born with a collodion membrane. Case: The Pediatric department consulted a 12 year old male with a chief complaint of itchy generalized scales on the body since birth. Patient also complained of bowing of lower limbs since 3-4years. According to the parent, at the time of birth, the patient was enveloped by membranes where the eyes could not close tightly. The patient was also unable to breastfeed. Physical examination showed ichthyosiform scales arranged lamellar in a mosaic pattern throughout the body. Histopathological examination results support the diagnosis of congenital ichthyosiform erythroderma. The patient was given with injection vitamin D3 600000IU with calcium supplementation and calcitriol sachets, emollient and supportive therapy. A good improvement shown by markedly improvememt in bowing of limbs, scales and skin stiffness was seen after six weeks of treatment. Conclusion: Congenital ichthyosiform erythroderma is a rare type of ichthyosis. Treatment aims to prevent excessive transepidermal water loss, prevent complications such as rickets, pathological fractures and to reduce clinical symptoms.
Keywords
Congenital ichthyosiform erythroderma, Transepidermal, Calcitriol sachets.
Introduction
Ichthyosis is a heterogeneous group of skin disorders characterized by generalized scales and dryness. Scales signify changes in epidermal differentiation [1,2]. Clinical symptoms of Ichthyosis depend on aetiology. Ichthyosis is divided into three subgroups: Autosomal dominant ichthyosis, X-linked recessive ichthyosis and autosomal recessive ichthyosis [3,4].
Congenital Ichthyosiform Erythroderma (CIE) is an autosomal recessive Ichthyosis. CIE is the rarest disease that appears at birth, where the newborn infant is usually encased in a collodion membrane [1]. The prevalence of CSI is about 1 in 300,000 births. Ichthyosis is twice more common in men. Twenty-five percent of patients were born premature, and in 51% of cases, the siblings are also affected with CIE. In some patients, the disease is limited to the trunk and extremities while in eighty percent of cases a systemic involvement is found [4]. A genetic defect in TGM 1 gene is the basis of CIE, where this gene mutation is found in 50% of patients. 2 TGM 1 gene encodes transglutaminase 1, ALOX12B, ALOXE3, an enzyme that is crucial in the formation of envelope cells in keratinocyte differentiation [6].
Diagnosis is based on clinical symptoms, family history, and can be supported by morphological examination and other specialized tests. If available, molecular analysis is recommended to confirm the diagnosis. This test is also useful for family member testing and prenatal diagnosis. A routine histopathological finding in some Ichthyosis is not characteristic, often only showing only epidermal hyperplasia and varying degree of ortho-hyperkeratosis. In combination with typical clinical findings, the result of histopathological examination can provide important clues to Ichthyosis vulgaris or Ichthyosis epidermolysis [7]. We report a case of CIE in a 12 year old male with a history of generalized scales since birth and progressive genu valgum deformity. The objective of this report is to describe the clinical features and complications of CIE as well as the current treatment options.
Case Study
A 12-year-old male presented to the department of paediatrics of ananta medical college and research centre, Udaipur-Rajasthan, India department with a chief complaint of generalized scales since birth. Pruritus was present which was exacerbated during perspiration and hot environment. The scales were persistent and never subsided. There was associated bowing of legs for the past 3-4 years. He was born out of non-consanguineous marriage as an appropriate for gestational age baby. According to the parents, the baby was born bright red with few vesico-bullous lesions over the body. These lesions gradually increased over 1-2 years, being prominent at sites of friction where the skin underwent erosion, peeling and widespread denudation without scarring. Subsequently the bullae and erythroderma subsided but the skin became dry, thick, warty, and scaly with recurrent skin infections. None of his family members have similar issues
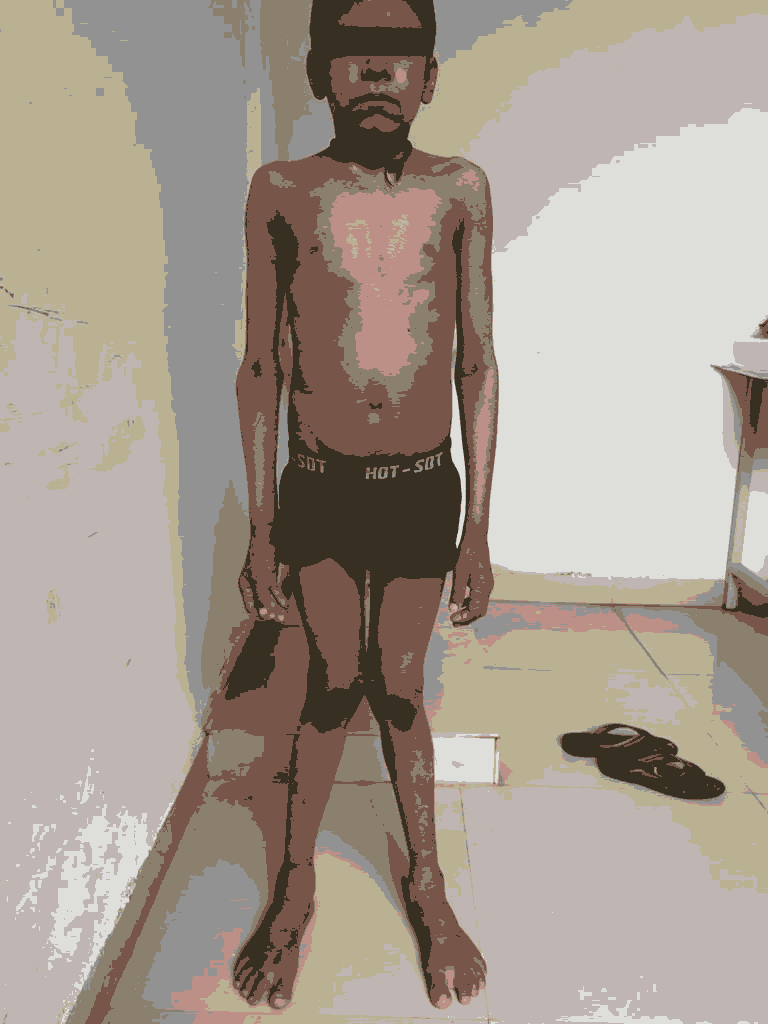
On examination, there was hyperkeratotic, scaly, warty, plaque like lesions over his extremities with relative sparing of the face, neck, palms and soles (Figure 1).
The lesions had nonhystrix brown scales. Mucosae, teeth and hair were normal. Along with this, the child had genu valgum, bowing of legs and widening of the wrists (Figure 2).
Examination of the chest, abdomen and central nervous system did not reveal any abnormality.
Laboratory examination revealed normal complete hemogram, peripheral bloodsmear examination, renal and liver function tests. Serum calcium was 8.32 mg/dl (normal 9–11 mg/dl), serum phosphorus was 3.42 mg/dl (normal 2.5–5.5 mg/dl) and serum alkaline phosphatase was 682.1 u/L (normal 250–650 u/L), 25-hydroxy Vitamin D level was 3.76 ng/ml (30–100 ng/ml) and X-rays of the knee and wrist revealed marked splaying, fraying and cupping of the distal metaphysis and widening of the growth plate (Figure 2). Hearing and vision assessment revealed no abnormality. Histopathological examination of skin biopsy showed mild ortho-keratosis and parakeratosis, there is elongation of rete pegs with fusion. Mild mononuclear inflammation is seen in perivascular location in superficial dermis.
In view of the above findings, a diagnosis of CIE with nutritional rickets was made and the child was started on parenteral Vitamin D3 (6 lakhs IU, intramuscular) and oral calcium supplementation (500 mg twice daily) for 6 months. Regular sun exposure for at least 20 min/day was advised, and white paraffin was advised for the skin lesions. Follow-up after 3 months revealed marked improvement in the radiological findings, normal serum calcium (10.6 mg/dl), phosphorus (5.2 mg/dl), alkaline phosphatase (115 u/L), and 25-hydroxy-vitamin D3 (46 ng/ml) but minimal change in the skin condition.
Discussion
In this case, a 12 year old boy came with a chief complaint of generalized scales since birth. The patient was born with a thick membrane, and the skin was dry and hard. Pruritus was some- times present. This clinical finding is consistent with CIE, which is an autosomal recessive disorder due to TGM 1 gene mutation that encodes for transglutaminase me. According to the literature, infants with CIE are usually born with generalized scales since birth. They are typically born with hard parchment-like membrane during the first week of life. Initially, the skin appears to be erythematous which with time hardens and forms mosaic- pattern scales [1,2,9]. It then develops into a shiny, dry, and brownish yellow structure, resembling a parchment membrane [2]. The physical examination showed generalized ichthyosiform lamellar scales with a mosaic pattern, fissures, and erosions.
In children with various forms of ichthyosis, rickets may develop due to defective synthesis of Vitamin D owing to diseased epidermis or loss of calcium through skin, leading to elevated parathormone levels and low Vitamin D3 levels as postulated by Milstone et al. [17]. Although rickets have been described in association with lamellar ichthyosis and X-linked ichthyosis, very few case reports in literature exist correlating rickets with EHK; one such reported by Perosa et al. in and two such from India too[18-20]. In a study of 41 Sudanese children with rickets attributed to vitamin D deficiency, 3 children were reported to have ichthyosis [21]. Factors associated may be poor penetration of sunlight owing to keratinocyte proliferation, increased cholesterol catabolism involving vitamin D receptors, associated Vitamin D dependent rickets or less sun exposure [19].
Conclusion
The importance in identifying this disorder lies in the fact that CIE appears to be extremely refractory to treatment and in the majority of the cases lifelong vitamin D and calcium supplementation may be necessary. Although the rachitic features improved with supplementation of vitamin D and calcium, there was no improvement in the skin condition. This finding was similar to that observed by Thacher et al. [22]. Therefore in severe ichthyosis, evaluation should be done for rickets, especially in developing countries where there is a background of vitamin D deficiency to detect it at the earliest as such patients often need lifelong supplementation with vitamin D and calcium.
Acknowledgment
Department of paediatrics, Ananta medical college and hospitals, Udaipur, Rajasthan, India.
References
- Flekman P, DiGiovanna JJ. The ichthyoses fitzpatrick’s dermatologi in general medicine (8th edn). 2012; 49: 507-37.
- Dhabarde, Kavita AAH, Madan. A rare case report of lamellar ichtyiosis “collodion baby” with severe cicatri- cial ectropion in both eyes. IJSR 2015; 4: 148-50.
- Leonibus, Chiara De, Lembo, et al. Lamellar ichtyiosis and arthrogryposis in a premature neonate. J Dermatol Case Rep 2015; 2: 49-51.
- Alavi A, Shahshahani, Mostafa M, et al. Manifestation of diffuse yellowish keratoderma on the palms and soles in sutosomal recessive congenital ichtyio-sis patients may be indicative of mutations in nipal4. JDA 2011; 38: 1–7.
- Suraiyah, Soedibyo S, Boediardja SA. Lamellar Ichthyosis in Children with a History of Infant Colodion. Department of Skin and Sex, Department of Child Health Sciences, FKUI, Jakarta 2007;9: p 32-8
- . Huang JJ, Huang MY, Huang TY. Lamellar Ichtyiosis with Severe BLIateral Ectropion and Self-healing Collodion Mem-brane. Biomarkers and genomic medicine 2013; 5: 110-12.
- Oji V, Tadini G, Masashi A, et al. Revised nomenclature and classification of inherited ichthyoses: results of the first ichthyosis consensus conference in soreze 2009. J Am Acad Dermatol 2010; 63(4): 607-41.
- . Kumar S, Shailly R, Ifsa S, et al. BiIateral ectropion in a 3 months old baby with lamellar ichtyiosis: A rare case report. Int J Res Med Sci 2015; 3(9): 2443-5
- Shaik MdJ, Kumar SR, Barun PL, et al. Congenital lamellar ichthyosis in newborn: A case report. j of evidence based medicine and healthcare. 2015; 2(15): 2343-47.
- . Ryan O'Shaughnessy FL, Ishaan C, John IH, et al. Interleukin-1 alpha blockade prevents hyperker-atosis in an in vitro model of lamellar ichthyosis. Human Molecular Genetics 2010; 19(13): 2594–2605.
- Rodriguez RV, Stull C, Yosipovitch G. Chronic pruritus in the elderly: pathophysiology, diagnosis and management. J Drug Aging 2015; 32(3): 201-15.
- Faraji A, Mobaraki M, AmirReza Y, et al. A report of two cases of tgm1 mutations in iranian patients with lamellar ichthyosis. Iran J ChLId Neurology 2011; 5(1): 43-6.
- Aggarwal S, Rajan S. Lamellar ichtyiosis with severe bliateral ectropion. J K Practitioner 2014; 19: 60-2
- Reddy PK, Ravindra K. Lamellar Ichtyiosis: A rare case report. Ind J of Bas and Appl Med Res 2015; 4(2): 421-3.
- Pratyusha K, Sree PD, Reddy B. Successful outcome of lamellar ichtyiosis with oral retinoid therapy: A series of six cases. Indian J Paediatr Dermatol 2016; 17(2): 125-8.
- Pranitha V, Thimma RB, Daneswari V, et al. Lamellar icthyosis: A case report. J Clin Diagn Res 2014; 8(11): ZD01-2.
- Milstone LM, Ellison AF, Insogna KL. Serum parathyroid hormone level is elevated in some patients with disorders of keratinization. Arch Dermatol 1992; 128(7): 926-30.
- Perosa A, Sardella L, Acquafredda A, et al. Epidermolytic ichthyosis and rickets. Eur J Pediatr Dermatol 2004; 14(1): 13-6.
- Nayak S, Behera SK, Acharjya B, et al. Epidermolytic hyperkeratosis with rickets. Indian J Dermatol Venereol Leprol 2006; 72: 139-42.
- Sethuraman G, Khaitan BK, Dash SS, et al. Ichthyosiform erythroderma with rickets: Report of five cases. Br J Dermatol 2008; 158(3): 603-6.
- I el Hag AI, Karrar ZA. Nutritional vitamin D deficiency rickets in Sudanese children. Ann Trop Paediatr 1995; 15(1): 69-76.
- Thacher TD, Fischer PR, Pettifor JM, et al. Nutritional rickets in ichthyosis and response to calcipotriene. Pediatrics 2004; 114(1): e119-23.