Current Pediatric Research
International Journal of Pediatrics
Clinical and radiological profile of children with tuberculosis and their response to fixed dose combination anti-tubercular treatment.
K. Madhuri, Saswat Subhankar*, C.M. Rao, D.P. Dash
Department of Respiratory Medicine, Kalinga Institue of Medical Sciences, Odisha, India
- Corresponding Author:
- Saswat Subhankar
Department of Respiratory Medicine,
Kalinga Institue of Medical Sciences,
Odisha,
India
E-mail: saswat.kmc04@gmail.com
Received: 14 September, 2020, Manuscript No. AAJCP-24-19088; Editor assigned: 17 September, 2020, Pre QC No. AAJCP-24-19088 (PQ); Reviewed: 01 October, 2020, QC No. AAJCP-24-19088; Revised: 01 November, 2024, Manuscript No. AAJCP-24-19088 (R); Published: 29 November, 2024, DOI: 10.35841/0971-9032.28.11.2397-2401.
Tuberculosis (TB) is an important cause of morbidity and mortality in children especially in endemic countries. Childhood TB constitutes 10%-20% of all TB cases in high burden countries and accounts for 8%-20% of TB related deaths. Globally, nearly 1 million cases of TB and 2,33,000 TB related deaths occurred in children less than 15 years in 2018. Childhood TB reflects uncontrolled adult TB in a community.
Keywords
Tuberculosis, Childhood, Community, Morbidity.
Introduction
The diagnosis of tuberculosis in children is challenging due to various reasons like paucibacillary nature of tuberculous disease, difficulty in obtaining respiratory samples for examination and overlapping feature of tuberculosis with other common childhood infections like bronchiolitis, pneumonia, malnutrition and presence of HIV associated lung disease [1].
Children show higher predisposition to development of extrapulmonary TB because of higher rate of lymphohematogenous dissemination. Impact of extra pulmonary tuberculosis is greatest among infants and young children as they tend to develop severe extrapulmonary disease, like meningitis and miliary TB. In approximately less than 40% cases in children, TB is microbiologically confirmed and in the remaining, diagnosis is made by other methods.
Multi drug regimen in Fixed Dose Combination (FDC) is used in treatment of childhood tuberculosis as this achieves treatment objectives, maximize treatment compliance and minimize drug toxicity. Duration of treatment depends on type and severity of tuberculosis. Clinical outcomes are usually better in children with TB than adults with mortality ranging from 0% and 2.2%. Mortality may be high in case of HIV coinfection [2].
The present study analyses the various types of clinical presentations of paediatric tuberculosis and the response to supervised anti tubercular treatment in these cases.
Aims and objectives
• To study the various types of presentations of tuberculosis
in the paediatric population and the outcome of FDC in
children ≤ 18 years of age.
• To describe clinical, radiological and microbiological
characteristics of paediatric patients with diagnosis of
tuberculosis.
Materials and Methods
The study was conducted in the Dept. of Respiratory Medicine and Department of Paediatrics, Kalinga Institute of Medical Sciences (KIMS), Bhubaneswar (BBSR) between October 2018 and March 2020 [3].
Study design
Prospective observational study.
Inclusion criteria
All newly diagnosed consecutive cases of pulmonary or extra pulmonary TB in children (<18 yrs) and initiated on supervised treatment were included in the study.
Exclusion criteria
• Children on anti-tubercular treatment for more than 1
month.
• Inability to obtain consent from guardian (in case of
children ≤ 14 years of age) or patient himself/herself (for
children >14 years of age).
Procedure
After proper counselling and obtaining valid consent, all new consecutive cases of tuberculosis (pulmonary and extrapulmonary) diagnosed either microbiologically or clinically in children ≤ 18 years of age were included in the study.
A detailed history of the patient along with a complete physical examination and routine investigations were performed for all patients and recorded in a proforma [4]. Follow-up of all cases was done at the end of Intensive Phase (IP) and at the end of treatment. Improvement in general condition (in terms of symptoms, signs and weight gain), tolerance to ATT and radiological improvement, sputum AFB status and adverse effects were recorded at follow-up. Each case was observed till completion of course of ATT and declared as “treatment completed” or “cured”. Children who were declared “transferred out” or “lost to follow up” were also recorded. Deaths were also recorded. All the cases were defined as per WHO guidelines.
The anti-tubercular regimens (FDC) were modified if needed based on patient tolerance and adverse reactions. The duration of treatment was extended whenever indicated [5].
Statistical analysis
The data collected was clubbed together in a single chart on MS Excel and represented in charts. Microsoft excel was used to draw charts. All statistical analysis was done using Graphpad calculator.
Results
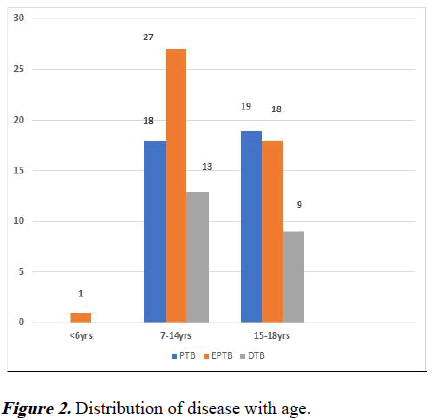
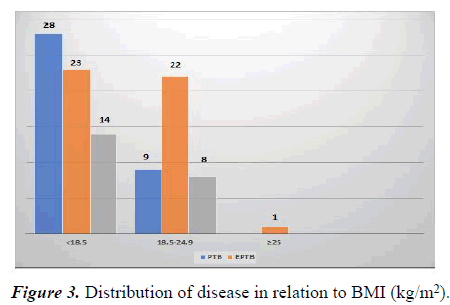
A total of 105 pediatric tuberculosis cases were included in our study out of which 59 were male (56.19%) and 46 female (43.8%). The mean age of the study group was 13.75 (± 2.98 yrs). The majority of cases belonged to the age group of 7-14 yrs. (58 cases; 55.2%) with 37 males and 21 females. Fever was the most common presenting complaint and was present in 66 cases (62.8%). This was followed by cough in 64 cases (60.9%) and glandular enlargement in 55 cases (52.3%). Generalised weakness was the most common constitutional symptom and was present in 51.42% cases. The mean BMI in our study group was 17.48 (± 2.83 kg/m2); 65 cases (61.9%) had BMI less than 18.5 kg/m2 and 39 cases (37.14%) had a BMI between 18.5-24.9 kg/m2 (p=0.0003). Only 1 case had a BMI above 25 kg/m2 (p<0.0001) [6].
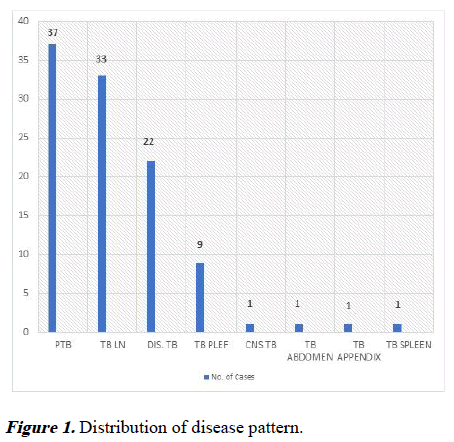
Pulmonary Tuberculosis (PTB) was diagnosed in 37 cases (35.2%). This was followed by TB lymphadenitis (33 cases, 31.4%) which included predominantly cervical in 28 cases (84.84%) and axillary group of lymphnode in 5 cases (15.15%) (Figure 1). Majority of the cases diagnosed with EPTB belonged to the age group of 7-14 years (Figure 2). Disseminated TB and pleural effusion were reported in 20% and 8.57% cases respectively. 1 case each of CNS TB, miliary TB, TB abdomen, TB appendix and TB spleen were recorded.
The no. of cases were maximum in children who had a BMI of less than 18.5 kg/m2 (61.9%) with 28 cases of PTB. The no. of disseminated TB cases were also highest in this group (13.3%) (Figure 3) [7].
A total of 119 samples were collected of which sputum (53.3%) and FNAC/biopsy (41.9%) were the commonest. Microbiological confirmation could be obtained only in 53 (50.47%) cases that included 24 cases of PTB and 29 EPTB cases. The remaining cases were clinically diagnosed with radiology assisting the diagnosis in 25 (23.8%) cases, FNAC or biopsy in 17 (16.19%) and body fluid analysis in the remaining 10 (9.52%) cases (Table 1) [8].
| Investigation | PTB | % | EPTB | % | Total |
|---|---|---|---|---|---|
| Microbiologically confirmed | 24 | 22.85% | 29 | 27.61% | 53 |
| Clinically diagnosed | |||||
| Radiology | 13 | 12.38% | 12 | - | 25 |
| FNAC/Biopsy | - | - | 17 | 16.19% | 17 |
| Body fluid analysis | - | - | 10 | 9.52% | 10 |
Table 1. Investigations assisting in diagnosis.
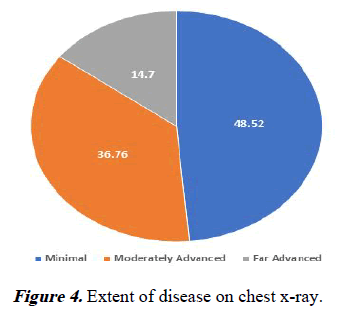
In patients diagnosed clinically, chest X-ray was the most commonly used. Chest X ray finding was present in 64.76% (68 cases) out of which infiltration and consolidation were the most common finding (20 cases each; 29.4% each) followed by pleural effusion in 19.11%. Cavitary lesions were seen in 14.7%, hilar lymphnode enlargement in 10.29%, nodular shadows in 7.35%, paratracheal widening in 7.35%. Segmental collapse was noted in 1 case. Extent of disease in a chest x-ray film can be graded as minimal, moderately advanced, far advanced lesions (Figure 4). Hematotological disturbances were commonly reported in the study group. The mean hemoglobin, RBC count, MCV, MCH and MCHC were detected to be lower than normal. The albumin to globulin ratio was also lower than normal (Table 2) [9].
| Parameter | Mean value | S.D |
|---|---|---|
| TLC (cells/µl) | 7871.83 | 3024.22 |
| Hemoglobin (mg/dl)* | 9.72 | 1.96 |
| RBC (/µl) | 4.42 | 0.88 |
| MCV (fl/µm3)* | 70.5 | 10.68 |
| MCH (pg)* | 22.18 | 3.52 |
| MCHC (g/dl)* | 31.14 | 1.5 |
| Platelet count (µl) | 3,60,000 | 1.3 |
| FBS (g/dl) | 95.39 | 19.12 |
| Albumin:globulin* | 0.98 | 0.28 |
| Urea (mg/dl) | 15.27 | 4.21 |
| Creatinine (mg/dl) | 0.51 | 0.14 |
Table 2. Blood investigations.
All the cases were followed up at the end of IP and then at the end of CP. During the IP, 5 patients transferred out. As many as 93 (88.57%) of the remaining patients reported symptomatic improvement and weight gain was recorded in 77 (73.3%). 60 (57.14%) children showed evidence of radiological improvement.
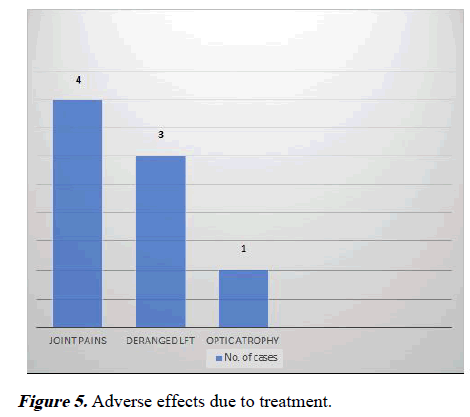
During CP, 7 patients transferred out and the remaining 93 (88.57%) were declared “treatment completed” or “cured”. This included 13 patients who required extension of CP. Weight gain was recorded in 76 (81.72%) patients. Joint pain and a derangement in liver function test were the most common adverse effects recorded (4 cases; 3.8% each) (Figure 5). However, only 3 of the cases required a change in the regimen while others improved with conservative management [10].
Discussion
Our study included 105 patients of which 59 were male (56.19%) and 46 were female (43.80%) with a M:F of 1.28:1. The WHO global report estimated the male to female ratio in children to be almost equal to 1. Similar results have also been seen in few other studies by Sreeramareddy et al. Socioeconomic and cultural factors leading to barriers in accessing health care may cause under notification in females. However, the increasing awareness of disease and attempts at reducing the stigma associated with it has improved the reporting of disease among women in recent times.
The mean age of patients in our study was 13.75 (± 2.98 yrs). Majority of patients belonged to the age group of 7-14. In a recent study by Ozden Turel et al., mean age of involvement was 7.8 years. The mean age in this study of population was higher as there was only 1 case below the age of 6 years and no case below the age of 5 years.
Clinical presentation in children with TB may be varied, thus posing a problem in diagnosis. In our study, fever was the most common presenting complaint in (62.8%) followed by cough (60.9%) and glandular enlargement (52.3%). In the study by Sreeramareddy et al. fever, cough and lymphnode swelling were the most common presenting complaints. In a study by Loh SW et al., fever, cough and weight loss were the most common presenting complaints.
Majority of cases in our study had a BMI less than 18 kg/ m2 (65 cases; 61.9%). Pallor was detected on general physical examination of the patients in 61.9% cases. Malnutrition is prevalent in developing countries which may predispose to infection. Although the association of TB and BMI in children is not very well defined, it has been very much studied in adults.
Sputum samples could be collected from 56 (53.3%). This could be possible as 46 (43.8%) patients were above 15 years of age and were able to give sputum sample. 58 (55.2%) patients were between 7-14 years age group and of them many belonging to the upper age limit were able to give sputum samples. Sputum collection is a major problem in young children and examination of gastric aspirate in them helps.
Sputum for AFB was positive in only 22.85% cases in our study. In a study by Blount et al., AFB smear and mycobacterial cultures were positive in 18% and 21% cases respectively. In a study by OzdenTurel et al., AFB staining was positive in 13.1% cases and culture was positive in 18.7% cases.
Hematological abnormalities are common in TB. A study by Abay et al., in Northwest Ethiopia reported anaemia in 46%, neutropenia in 22% and thrombocytopenia in 8%. Similarly Singh et al., reported anaemia in 86% patients with PTB and in 84% with disseminated/miliary disease; other presentations include monocytopenia, leucocytosis and lymphocytosis or lymphopenia. Various pathogeneses have been suggested in TB associated anemia, but most studies have showed infection of the hematopoietic progenitor cells, effect of treatment on erythropoiesis and folate activity, nutritional deficiencies and malabsorption, absence or depletion of bone marrow iron and suppression of erythropoiesis by inflammatory mediators as the potential explanation.
FNAC of lymph node was performed in 42 cases from which microbiological confirmation was obtained from 66.7%. Bacteriological confirmation could be done in these cases as it is a tertiary care hospital with all available facilities.
Chest radiography is very useful in the diagnosis of TB in children as most cases have radiographic changes. In our study, chest X-ray finding was present in 64.76% and infiltration and consolidation (29.4% each) were the commonest findings.
Together with parenchymal opacities, hilar node enlargement was observed in 10.29% patients. In a study by Sreeramareddy et al., chest X-ray finding was present in 94% of PTB patients and 63% of EPTB patients. In a study by Basteiro et al., infiltration was the commonest finding on chest X-ray. In another retrospective study of chest X-rays in children with TB done by Kim et al., air-space consolidation was the commonest finding (80%).
70%-80% children are estimated to have disease in the lungs. However, when compared to adults, they have a higher chance of developing EPTB. In a study by Jain et al., 12% children were confirmed to have PTB while 56% had EPTB. Mazta et al., in their study reported PTB in 55% cases while 45% were diagnosed with EPTB.
Pulmonary tuberculosis was diagnosed in 37 cases (35.2%) in our study. Among patients with EPTB, TB lymphadenitis was the commonest (31.4%). Cervical group of lymphnodes were the most commonly affected followed by axillary group. This was in accordance with all the previously published reports. Disseminated tuberculosis was diagnosed in 20% (involving two or more noncontiguous organs). In a recent study by Aketi et al., 29% of children had smear negative PTB, 14.1% cases had smear positive PTB and 56.1% had EPTB. Nearly 74.2% cases of EPTB were TB lymphadenitis.
Disseminated TB is common in young children, usually less than 3 years old. The study group in our case had only 1 case less than 6 years of age who presented with CNS TB.
Treatment outcomes in children are generally favourable, provided treatment is started promptly and adherence is maintained. In a study by Aketi et al., 59% cases had completed course of treatment and only 2.5% had failed treatment. Mortality may be higher in cases of disseminated disease. The risk of adverse reactions is also very low in children.
Conclusion
TB in children is a major public health problem as it serves as a marker for recent transmission of TB. It is a major cause of disease, both pulmonary and extrapulmonary and death in young children, especially in endemic countries. The maximum number of cases among children occurs in children less than 5 years of age or more than 10 years of age. Infants, young children and immunocompromised children are more likely to develop life threatening forms of disease when compared to adults or adolescents.
The diagnosis of TB in children is difficult in most cases due to the difficulties in collecting specimens as well as because of the paucibacillary nature of the disease. Since a microbiological confirmation may not be possible in many cases, a combination of contact history, clinical signs and symptoms and radiological findings may help reach a diagnosis. Treatment outcomes in children are generally good if treatment is started early and adherence is maintained. The risk of serious adverse events in children associated with use of the recommended treatment regimens is also very low.
Children, their parents, other family members and other caregivers should be educated about TB and the importance of completing treatment. The support of the child's parents and immediate family is vital to ensure a satisfactory outcome of treatment.
References
- Sreeramareddy CT, Ramakrishnareddy N, Shah RK, et al. Clinico-epidemiological profile and diagnostic procedures of pediatric tuberculosis in a tertiary care hospital of western Nepal-a case-series analysis. BMC Pediatr 2010; 10: 1-7.
[Crossref] [Google Scholar] [PubMed]
- Blount RJ, Tran B, Jarlsberg LG, et al. Childhood tuberculosis in northern Viet Nam: A review of 103 cases. PloS One 2014; 9: e97267.
[Crossref] [Google Scholar] [PubMed]
- Aketi L, Kashongwe Z, Kinsiona C, et al. Childhood tuberculosis in a sub-Saharan tertiary facility: Epidemiology and factors associated with treatment outcome. PloS One 2016; 11: e0153914.
[Crossref] [Google Scholar] [PubMed]
- Turel O, Kazanci S, Gonen I, et al. Paediatric tuberculosis at a referral hospital in Istanbul: Analysis of 250 cases. Biomed Res Int 2016; 2016: 6896279.
[Crossref] [Google Scholar] [PubMed]
- Loh SW, Thoon KC, Tan NW, et al. Paediatric tuberculosis in Singapore: A retrospective review. BMJ Paediatr Open 2018; 2: e000308.
[Crossref] [Google Scholar] [PubMed]
- Abay F, Yalew A, Shibabaw A, et al. Hematological abnormalities of pulmonary tuberculosis patients with and without HIV at the university of Gondar hospital, Northwest Ethiopia: A comparative cross‐sectional study. Tuberc Res Treat 2018; 2018: 5740951.
[Crossref] [Google Scholar] [PubMed]
- Singh KJ, Ahluwalia G, Sharma SK, et al. Significance of haematological manifestations in patients with tuberculosis. J Assoc Physicians India 2001; 49: 788-790.
[Google Scholar] [PubMed]
- Garcia-Basteiro AL, Lopez-Varela E, Augusto OJ, et al. Radiological findings in young children investigated for tuberculosis in Mozambique. PLoS One 2015; 10: e0127323.
[Crossref] [Google Scholar] [PubMed]
- Kim WS, Moon WK, Kim IO, et al. Pulmonary tuberculosis in children: Evaluation with CT. AJR Am J Roentgenol 1997; 168: 1005-1009.
[Crossref] [Google Scholar] [PubMed]
- Jain SK, Ordonez A, Kinikar A, et al. Pediatric tuberculosis in young children in India: A prospective study. BioMed research international 2013; 2013: 783698.
[Crossref] [Google Scholar] [PubMed]