Current Pediatric Research
International Journal of Pediatrics
Biermer's disease reveled by iron-deficiency anemia in a child: A case report and literature review.
Lotfi Rahal1,2*, Youcef Bouchedoub3,4, Nassima Rachedi5, Warda Imene Ziani5, Khaoula Azouz5
1 Department of Medicine, University of Bechar, Bechar 08000, Algeria
2 Department of Medicine, Public Hospital Establishment of Bechar, Bechar 08000, Algeria
3 Department of Medicine of Blida, University of Blida 01, Blida 09000, Algeria
4 Central Laboratories, Hospital Cancer Center of Blida, Blida 09000, Algeria
5 Immunology Laboratories, University Hospital of Blida, Blida 09000, Algeria
- Corresponding Author:
- Lotfi Rahal
Department of Medicine of Bechar
Public Hospital Establishment of Bechar-
Algeria Faculty of Medicine of Bechar
University of Bechar Algeria
Tel: (+213) 559566670
E-mail: dr.lotfirahal@univ-bechar.dz
Accepted date: 17th September, 2021
We report the case of a 13-year-old girl with no particular medical history who presented with an anemic syndrome with weight stagnation associated with epigastralgia and transit disorders. The blood count confirmed the presence of a hypochromic microcytic anemia, and digestive exploration by oeso-gastroduodenal endoscopy revealed gastritis. The biopsy with histological analyses has revealed a chronic atrophic gastritis in favor of Biermer's disease. The Helicobacter pylori test was negative. The immunological exploration found a high level of anti-parietal cell antibodies confirming the diagnosis of Biermer's disease. Poorly described in children, Biermer's disease presents in our case a particular form due to the atypical clinical presentation different from the usual form described in the literature which usually associated macrocytic anemia and vitamin B12 deficiency.
Keywords
Case report, Biermer's disease, Microcytic anemia, Chronic gastritis, Vitamin B12.
Introduction
Biermer's disease is an autoimmune disease characterized by the presence of autoantibodies against parietal cells of the stomach and/or intrinsic factor inducing a deficiency in the latter leading to malabsorption of vitamin B12 or cobalamin [1,2]. This disease represents 20% to 50% of the etiologies of vitamin B12 deficiency in adults [3]. However, Biermer's disease remains rare in the pediatric population, only a few cases have been reported in the literature in pediatric patients [4-6]. The expressions of vitamin B12 deficiency are polymorphic and atypical, ranging from macrocytic anemia, hyper segmentation of neutrophils, neurological affection of the sensitive polyneuritis type to more advanced cases with marrow sclerosis and pancytopenia [7].
We report the case of a teenager who presented with a clinical picture of iron deficiency anemia that incidentally revealed a beginning Biermer's disease.
Case Report
Clinical history
A 13-year-old girl from eastern Algeria, with no particular pathological history, presented with chronic anemia (diagnosed 3 years ago) associated with asthenia, epigastralgia, transit disorders and weight loss. The clinical examination reveals a cutaneous-mucosal pallor and fragility of the phaneras. The questioning did not reveal any nutritional deficiencies or digestive or gynecological bleeding in this patient. The biological tests showed aregenerative hypochromic microcytic anemia (hemoglobin: 7.5 g/dl, n: 11.1-14.7 g/dl; mean corpuscular volume GMV: 67.1 fl, n: 75-95 fl; mean corpuscular hemoglobin concentration MCHC: 27.9 g/dl, n: 31-37 g/dl; reticulocytes: 51.103/mm3, n: 80.103-120.103/mm3), leukocyte and platelet levels are normal.
Hemoglobin (Hb) electrophoresis found a decrease in Hb A2 (1.8%, n: 2.2%-3.2%), supplemented by serum iron and serum ferritin tests that came back in favor of an iron deficiency anemia (Ferritinemia: 7 ng/mL, n: 8.8-184 ng/mL; serum iron: 0.12 mg/L, n: 0.4-1.5 mg/L). A biological evaluation of the nutritional status (Albuminemia: 38 g/L, n: 30-50 g/L; total protein: 77.44 g/L, n: 57-80 g/L), allowed to exclude an undernutrition at the origin of the iron deficiency anemia in this teenager.
The digestive signs associated with weight stagnation led us to perform an anti-transglutaminase antibody assay by ELISA, which was negative (anti-transglutaminase (tTG) IgG and IgA?4 U/mL), and a weighted serum IgA assay also normal (serum IgA: 1.48 g/L, n: 0.58-3.58 g/L), eliminating celiac disease.
Additional investigations
An esophageal endoscopy with biopsy was also performed showing a congestive gastric mucosa and an edematous duodenal mucosa, lined with a whitish staining in favor of bulbo-duodenitis.
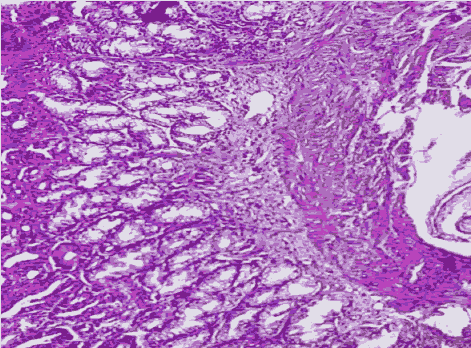
The histological analyses examination of the biopsy fragments was in favor of a chronic gastritis with moderate intensity and atrophy without signs of Helicobacter pylori HP infection, nor of metaplasia or dysplasia with the presence of two lymphoid clusters compatible with a Biermer’s disease (Figure 1). In the duodenum, lymphocytic infiltration was estimated to be 10%-20% locally.
The research of autoantibodies against gastric parietal cells came back strongly positive (equal to 1/80th) on triple substrate (liver, kidney and rat stomach). Nevertheless, the vitamin B12 levels were normal (376 pg/mL, n: 190-950 pg/mL).
The diagnosis of Biermer's disease in this adolescent girl was retained in view of the presence of histological criteria of chronic atrophic gastritis with lymphocytic inflammatory infiltrate and absence of HP infection. And criteria of autoimmunity marked by the presence of autoantibodies against gastric parietal cells.
Discussion
Biermer's disease is an autoimmune disorder characterized by atrophic gastritis which is responsible for a defect in the secretion of intrinsic factor by the gastric parietal cells leading to malabsorption of vitamin B12 which is the cause of the hematological manifestations [8]. Vitamin B12 or cobalamin is a hydrosoluble vitamin that plays an important role in hematopoiesis and the development of the nervous system [9]. It is provided exclusively by the food supply and is mainly found in animal products such as meat, fish, eggs and dairy products. In the duodenum and jejunum this vitamin is linked to the intrinsic factor produced by the fundus parietal cells and the body of the stomach, which also promotes the absorption of vitamin B12 in the terminal ileum [10].
Part of the vitamin B12 is stored in the liver (2 to 3 mg), these stocks allow to cover the needs in vitamin B12 during the deficits of contribution for a 2 to 4 years duration [11]. The hematological manifestations are classically characterized by an aregenative macrocytic anemia with medullary megaloblastosis, pancytopenia, morphological abnormalities of platelets, and neutrophilic polynuclei [12], however, these manifestations remain mostly atypical both clinically and biologically with a usually insidious beginning [13].
Biermer's disease manifests mainly in adults over 60 years of age [14], it remains rare in young people and children and is exceptional in infants [15]. Its main mechanism is based on the presence of autoantibodies against parietal cells leading to an alteration in the functioning of the cells responsible for acid secretion (alteration of the proton pump) and gastric atrophy leading to a deficit in the synthesis of intrinsic factor and to achlorhydria. These two consequences are the causes of vitamin B12 deficiency by malabsorption and iron deficiency because the latter requires gastric acidity to be converted into soluble ferrous iron that is easily absorbed by the intestinal mucosa. In the rare cases of Biermer's disease in the pediatric population reported in the literature, the clinical presentation of this pathology was atypical and in rare cases Biermer's disease presented with the usual forms of macrocytosis and neurological impairment. A female predominance has been found in children with this condition in the various cases reported in the literature [16].
Thus, Serraj et al reported the case of a 15-year-old girl who presented a severe hematological disorde revealing a vitamin B12 deficiency with an acute hemolytic anemia associated with ascites; the clinical presentation associated a vitamin B12 deficiency, a hemolytic anemia, thrombocytopenia, fever and a renal failure giving the aspect of a thrombotic microangiopathy [6]. In another study, Cariou et al reported the case of a five-month-old exclusively breastfed infant who presented a Vitamin B12 deficiency associated with methylmalonicaciduria, as well as weight and psychomotor retardation; this vitamin deficiency was the consequence of an unrecognized maternal Biermer disease [4]. Biermer's disease in children can present in several clinical and biological forms, it can be normocytic or macrocytic, as well as isolated or associated with pancytopenia, as in the case reported by Amrani et al. in an adolescent girl where Biermer's disease was revealed by repeated epistaxis and a pronounced anemic syndrome associated with a growth delay and digestive symptoms; The haemogram showed pancytopenia, severe hypochromic macrocytic anemia and leuko-neutropenia with thrombocytopenia [17].
One of the complications of achlorhydria in Biermer's disease is martial deficiency; the association of Biermer's disease with iron deficiency anemia has been described in adults in several studies, but remains uncommon in children. The study by Zulfiqar et al. which found a martial deficiency in 29% of subjects with Biermer’s disease (42 subjects), this deficiency affected essentially young female subjects [18]. This association with a female predominance was also found in other studies, notably by Lagarde et al. and Marignani et al. [19,20].
Although presenting a Biermer’s disease, our patient did not have a deficiency in vitamin B12 nor neurological signs that can be explained by the early diagnosis of this disease and the persistence of stock of vitamin B12 still covering the needs of the organism. This requires a clinical and biological monitoring with periodic measurements of vitamin B12 levels, intrinsic factor, a complete blood count and the realization of control endoscopy in order to follow the evolution of the disease and to detect complications related to Biermer’s disease.
Conclusion
Biermer's disease is a rare pathology in children and can present in many atypical forms. In the absence of a clear etiology, chronic iron deficiency anemia in children associated with digestive signs should require specialized investigations in order to detect a possible gastric disorder caused by a dysfunction of the parietal cells responsible for both Biermer's disease and a defect in iron absorption leading to associated iron deficiency anemia.
Data Availability
No data were used to support this case report.
Consent
Written informed consent for publication was taken from the patient.
Authors’ Contributions
Rahal L: Disease diagnosis and patient follow-up, study design and manuscript writing; Bouchedoub Y: Study design and conception, analysis and interpretation of results and critical revision. Rachedi N, Ziani I, Azouz K: Immunological analyses.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- Andres E, Serraj K. Optimal management of pernicious anemia. J Blood Med 2012; (3): 97-103.
- Annibale B, Lahner E, Fave GD. Diagnosis and management of pernicious anemia. Curr Gastroenterol Rep 2011; 13(6): 518-24.
- Loukili NH, Noel E, Blaison G, et al. Current data on Biermer's disease. About a retrospective study of 49 observations. Update of pernicious anemia. A retrospective study of 49 cases. Rev Med Interne 2004; 25(8): 556-61.
- Cariou M, Joncquez A, Prades N. Vitamin B12 deficiency in a five-month-old infant: A case report. Immuno-analysis and specialized biology 2013; 28(2-3): 133–136.
- Mathey C, Di Marco JN, Poujol A, et al. Weight stagnation and psychomotor regression revealing vitamin B12 deficiency in 3 infants. Arch Pediatr 2007; 669(5): 467-71.
- Serraj K, Housni B, Fothergill, et al. Biermer's disease in 15-year-old girl revealed by acute massive hemolytic anemia and ascites. JCC Open 2013; 25(1): 1-3.
- Serraj K, Mecili M, Andrès E. Signs and symptoms of vitamin B12 deficiency: a critical review of the literature. Médecine Thérapeutique 2010; 16(1): 13-20.
- Nafil H, Tazi I, Mahmal L. Biermer's disease and autoimmune hemolytic anemia. Ann Biol Clin 2012; 70(4): 480-2.
- Khellaf S, Boulefkhad A, Boudraa B, et al. Nervous system and cobalamin deficiency. Curr Res Psychiatry Brain Disord 2019: CRPBD-100005.
- Dainese-Plichon R, Hébuterne H. Digestion and absorption of nutrients in the small intestine. EMC-Gastroenterology 2012; 7(4): 1-14.
- Hariz A, Bhattacharya PT. Megaloblastic anemia. In: Statpearls. Treasure Island (FL): Stat Pearls Publishing 2020.
- Bizzaro N, Antico A. Diagnosis and classification of pernicious anemia. Autoimmun Rev 2014; 13(4-5): 565-8.
- Saint-Leger P, Barbare JC, Dupas JL, et al. Biermer's disease and microcytic anemia. Gastroenterol Clin Biol 2008; 1319(4)32: 363-438.
- Andres E, Serraj K. Optimal management of pernicious anemia. J Blood Med 2012; 6(3): 97-103.
- Cariou ME, Joncquez AL, Prades N, et al. Vitamin B12 deficiency in a five-month-old infant: about a case report. Immuno Anal BiolSpé 2013; 14(28): 133-136.
- Hershko C, Ronson A, Souroujon M, et al. Variable hematologic presentation of autoimmune gastritis: Age-related progression from iron deficiency to cobalamin depletion. Blood. 2006; 107(4): 1673-9.
- Amrani R, Es-seddiki A, Messaoudi S, et al. Biermer's disease: A rare entity in pediatrics. Revue marocaine de santépublique 2014; 20(1): 1.
- Zulphiqar AA, Dramé M, Pennaforte JL, et al. Martial deficiency and Biermer's disease: A rare association?. Ann Biol Clin. 2015; 15(73): 420-6.
- Lagarde S, Jovenin N, Diebold MD, et al. Is there any relationship between pernicious anemia and iron deficiency? GastroenterolClinBiol 2006; 30(11): 1245-9.
- Marignani M, Delle Fave G, Mecarocci S, et al. High prevalence of atrophic body gastritis in patients with unexplained microcytic and macrocytic anemia: A prospective screening study. Am J Gastroenterol 1999; 94(3): 766-72.