Current Pediatric Research
International Journal of Pediatrics
Barriers of breastfeeding in the first year of life: An assessment study.
Elham Atef Abdelazeem1*, Wafaa El Sayed Ouda2, Safaa Salah Ismail3
1Department of Pediatric Nursing, Sohag University, Sohag, Egypt
2Department of Pediatric Nursing, Ain Shams University, Cairo, Egypt
3Department of Pediatric Nursing, Helwan University, Cairo, Egypt
- *Corresponding Author:
- Elham Atef Abdelazeem
Department of Pediatric Nursing
Sohag University
Egypt
E-mail: elhamhosssam@gmail.com
Received: 25 November, 2022, Manuscript No. AAJCP-22-83224; Editor assigned: 28 November, 2022, Pre QC No. AAJCP-22-83224(PQ); Reviewed: 05 December, 2022, QC No. AAJCP-22-83224; Revised: 22 December, 2022, Manuscript No. AAJCP-22-83224(R); Published: 30 December, 2022, DOI:10.35841/0971-9032.26.12.1719-1729.
Background: Breastfeeding is the usual way of providing infants with adequate, pollution free and sustainable nutrients needed for growth and development. Many mothers experience barriers to achieve their breastfeeding goals, leading to reduced rates of breastfeeding initiation and continuation.
Aim: Assess the barriers of breastfeeding in the first year of life.
Design: A descriptive research design was utilized to achieve the aim of this study.
Setting: The study was conducted at immunization outpatient clinic in Dar Salama Abdullah maternal and child health center in Sohag City.
Sample: A purposive sample of 120 mothers having infants from birth to 12 months old and not suffering from mental or physical diseases.
Tool: A structured interview questionnaire to collect data regarding characteristics of mothers and their infants, history of infant feeding, knowledge of mothers about breastfeeding and barriers of breastfeeding related to mothers and their infants.
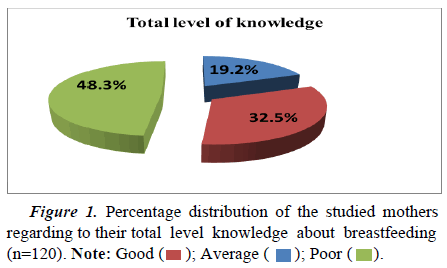
Results: Nearly half of the studied mothers have poor knowledge about breastfeeding and one third of them reported an average knowledge about breastfeeding and more than three quarters of them reported that premature infants, embarrassment from breastfeeding in public places and sore or cracked nipple were barriers to breastfeeding.
Conclusion: Most common barriers of breastfeeding related to mothers were pain during breastfeeding, sore or cracked nipples, breast engorgement, perception of insufficient milk supply, embarrassment from breastfeeding in public places, cesarean section, immunosuppressant’s, returning to work after delivery and breast cancer. Meanwhile the most common barriers related to infants were cleft lip, cleft palate, premature infants and breast refusal. Also, there were statistically significant differences between mothers’ barriers of breastfeeding and some of their characteristics. Recommendation: Early detection and adequate management of barriers hindering breastfeeding of infants in the first year of life.
Keywords
Barriers, Breastfeeding, Infant child
Introduction
Breastfeeding is the usual way of providing infants with adequate, pollution free and sustainable nutrients needed for growth and development [1]. Both WHO and UNICEF recommend early initiation of breastfeeding within 1 hour of birth, exclusive breastfeeding for the first 6 months of life and introduction of nutritionally adequate and safe complementary (solid) foods at 6 months together with continued breastfeeding up to 2 years of age or beyond. However, many infants and children do not receive optimal feeding [2].
Significant disparities in breastfeeding initiation and continuation remain based upon mothers’ demographic and socioeconomic status. Young, low-income, unmarried and less educated mothers have lower rates of breastfeeding. Disparitiesin continuation rates by maternal education indicated even steeper gaps. Socially and economically disadvantaged mothers face multiple barriers to breastfeeding as lack of information about the benefits of breastfeeding, receive limited or inadequate support from social support system, and lack jobs with maternal leave policies [3].
Promoting and supporting breastfeeding is an integral component of pediatric health care offered by Pediatric Nurse Practitioners (PNPs). As they promote informed choice about infant feeding practices by educating expectant parents, and their family members about the nutritional, neurodevelopmental, social and economic advantages of breast milk, educate families on the potential short and long-term health risks of not breastfeeding for both mother and infant and identify and reduce the actual and perceived barriers to initiation and continuation of breastfeeding at all phases of the childbearing/ childrearing cycle [4].
Significance of the study
Breastfeeding is one of the most effective global public health strategies to improve infant health and survival. Nearly 100% adherence to breastfeeding recommendations would save 820,000 children's lives per year and >$300 billion dollars annually [5]. Approximately 7.7% and 19.1% of all neonatal deaths may be avoided by the universal initiation of breastfeeding within the first day or first hour of life respectively [6]. Early detection and adequate management of lactational barriers and improving awareness about importance of breastfeeding could be reflected positively on the mothers and infants’ health [7].
Aim of the study
This study aimed to assess the barriers of breastfeeding in the first year of life.
Materials and Methods
Research design
A descriptive research design was utilized to achieve the aim of this study.
Research settings
This study was carried out at immunization outpatient clinic in Dar Salama Abdullah maternal and child health center in Sohag city. The building consists of two floors; ground floor that contains security room, hazardous waste room, meeting room, immunization clinic, family planning clinic, pregnancy clinic, pediatric clinic, the pharmacy, marriage clinic and the manager room. The first floor contains the laboratory, storeroom, bathrooms, nursing rooms, examining room, physician’s room and two inpatients’ departments for pediatric care.
Study subjects
A purposive sample of 120 infants and their accompanying mothers attending the above-mentioned setting were selected according to the following inclusion criteria:
Inclusion criteria:
Mothers regardless to their characteristics,
Infants not suffering from any mental or physical diseases,
Infants’ age: ranged from birth to 12 months old,
Both genders
Tools of data collection
One tool was used to achieve the aim of the study.
Tool I: Pre-designed questionnaire sheet (Appendix II): It was designed and written in an Arabic language by the researcher after reviewing the related literature. It consisted of 5 parts.
Part I: Characteristics of the mothers: It included 15 items related to:
Personal information: it included 7 items related to age, educational level, residence, social status, occupation, type of family and monthly income.
Reproductive history: it included 6 items related to number of pregnancies, birth interval, antenatal care follow up, counseling about breastfeeding during antenatal care, receiving support to start breastfeeding and kind of support.
Medical history of chronic diseases 2 items.
Part II: Characteristics of the infants: It included 7 items related to age, gender, birth weight, gestational age, birth order, and type of delivery and place of delivery.
Part III: History of infant feeding: It included 5 items related to initiation of breastfeeding, giving colostrum, giving prelactal feeds, type of feeding and time of giving external foods.
Part IV: Mothers' knowledge about breastfeeding: It included 16 items related to definition of exclusive breastfeeding, benefits of breastfeeding for infants, benefits of breastfeeding for mothers, benefits of breastfeeding for family, benefits of breastfeeding for society, breastfeeding positions, signs of good infant attachment, methods of acceleration after each feeding, signs of insufficient breast milk, factors that help to increase breast milk secretion, care provided for breast refusal, care provided for breast engorgement, care provided for mastitis, care provided for inverted nipples, mothers contraindications of breastfeeding, infants contraindications of breastfeeding and source of information about breastfeeding.
Scoring system: The total scores of the questions were 32 degree which equal 100%, each question was assigned a score according to mothers knowledge, responses were “good” if complete correct answer, “average” if incomplete correct answer, “poor” if select only one answer and were scored 2, 1 and 0 respectively. These scores were summed and were converted into a percent score. It was classified into 3 categories: good knowledge ≥70%, average knowledge from 50% to <70% and poor knowledge <50%.
Part V: Barriers of breastfeeding: It consisted of 2 parts as the following:
a) Barriers related to mothers: 1) Lactation barriers of breastfeeding (9 items): Pain during breastfeeding, sore or cracked nipples, inverted nipple, breast engorgement, plugged ducts, mastitis, breast abscess, leaking milk and low milk supply.
2) Psychological barriers to breastfeeding (8 items): Perception of insufficient milk supply, postnatal depression, embarrassment from breastfeeding in public places, lack of self-efficacy, lack of social support, lack of support from father, fear of distorted breast shape by breastfeeding and unpleasant odor of nursing mothers.
3) Obstetric and gynecological barriers to breastfeeding (6 items): Pain following vaginal or caesarean birth, caesarean section, postpartum fatigue, new pregnancy, twin delivery and taking contraceptives.
4) Drugs barriers to breastfeeding (6 items): Postoperative medications, anesthetics and analgesics drugs, antiepileptic drugs, immunosuppressant’s, opiates and their derivatives and chemotherapy.
5) General barriers to breastfeeding (9 items): Lack of knowledge about breastfeeding, returning to work after delivery, hospital policies and clinical practices, promotion and marketing of breast milk substitutes, maternal physical exhaustion, lack of personal freedom due to breastfeeding, radiotherapy and breast cancer.
b) Barriers related to infants: 1) Congenital barriers to breastfeeding (3 items): Cleft lip, cleft palate and tongue tie.
2) Health barriers to breastfeeding (8 items): Premature infants, Down syndrome, breast milk jaundice, poor sucking and swallowing reflexes, insufficient weight gain, infant thrush, breast refusal and poor latch on.
Scoring system: The total scores of the questions were 49 degree which equal 100%, each question was assigned a score according to mothers' response agree or disagree and were scored 1 and 0, respectively. These scores were summed and were converted into a percent score. It was classified into 3 categories: High barrier >70%, moderate barrier from 50% to <70% and low barrier <50%.
Content validity and reliability
It was ascertained by a group of experts in pediatric nursing professor. Their opinions elicited regarding the format, layout, consistency, accuracy and relevancy of the tools. Reliability analysis by measuring of internal consistency of the tool through Cronbach's alpha test was 0.788 for mothers’ knowledge of breastfeeding and Cronbach's alpha test was 0.802 for barriers of breastfeeding.
Pilot study
A pilot study was carried out on 10% of mothers to assess feasibility of the data collection tool as well as clarity and objectivity of the study tools, estimate the average time needed for data collection, add, or omit question, and to identify problems that might be encountered during implementation of the study. The mothers were included in the study sample because there were no radical modifications were done.
Fieldwork
Data were collected over a 6 months period, from the beginning of February 2020 to the middle of March 2020 andfrom the beginning of July to the middle of the November (due to stopping of data collection from 15/3/2020 to 30/6/2020 because of spread of COVID-19). The researcher was visiting the study setting 2 days/week (Saturday and Tuesday) from 8:30 am to 2 pm to collect data. Firstly, the researcher met the mothers in the previously mentioned setting, and then started by introducing herself to each mother, giving a clear and brief idea about the aim of the study and its expectations. Secondly, individual interviewing was done after obtaining verbal consent from the mothers to participate in the study. The questionnaire was filled by researcher which took about 30-35 minutes.
Administrative design
A letter was issued from dean of the faculty of nursing, Helwan University to the director of Dar Salama Abdullah maternal and child health center at Sohag city for explaining the aim of the study to obtain their permission and cooperation. The researcher met the director of Dar Salama Abdullah maternal and child health center at Sohag city to explain the purpose and the methods of the data collection and an official permission to conduct the study was obtained.
Statistical analysis
Data collected from the studied sample was revised, coded, and entered using Personal Computer (PC). Computerized data entry and statistical analysis were done using the Statistical Package for Social Sciences (SPSS) version 22. Data were presented using descriptive statistics in the form of frequencies, percentages. Chi-square test (χ2) was used for comparisons between qualitative variables. Spearman correlation measures the strength and direction of association between two ranked variables.
Significance of the results
• Highly significant at p-value<0.01.
• Statistically significant was considered at p-value<0.05.
Results
Table 1 revealed that more than half (53.3%) of the studied mothers were between 25 and less than 30 years old ( ± SD 27.5 ± 5.98), most (83.3%) of mothers were married, more than half (52.5%) of them were housewife, nearly two thirds (65.8%) lived in extended family type and more than two thirds (70%) of them had un-enough monthly income.
| Personal information | No | % |
|---|---|---|
| Age | ||
| 20<25 | 23 | 19.2 |
| 25<30 | 64 | 53.3 |
| 30<35 | 19 | 15.8 |
| 35 ≤ 40 | 14 | 11.7 |
| ± SD 27.5 ± 5.98 | ||
| Social status | ||
| Married | 100 | 83.3 |
| Divorced | 17 | 14.2 |
| Widow | 3 | 2.5 |
| Occupation | ||
| Working | 57 | 47.5 |
| Housewife | 63 | 52.5 |
| Type of family | ||
| Nuclear | 41 | 34.2 |
| Extended | 79 | 65.8 |
| Monthly income | ||
| Enough | 36 | 30 |
| Not enough | 84 | 70 |
Table 1. Number and percentage distribution of the studied mothers regarding to their characteristics (n=120).
Figure 1 showed that nearly half (48.3%) of the studied mothers had poor knowledge about breastfeeding. On the other side, only 19.2% of them had good knowledge and less than one third (32.5%) of them had average knowledge about breastfeeding.
Table 2 demonstrated that 63.3%, 75.8% and 68.3% of the studied mothers agreed that pain during breastfeeding, sore or cracked nipples and breast engorgement are barriers of breastfeeding respectively.
| Items | Agree | Disagree | ||
|---|---|---|---|---|
| No | % | No | % | |
| Pain during breastfeeding | 76 | 63.3 | 44 | 36.7 |
| Sore or cracked nipples | 91 | 75.8 | 29 | 24.2 |
| Inverted nipples | 60 | 50 | 60 | 50 |
| Breast engorgement | 82 | 68.3 | 38 | 31.7 |
| Plugged ducts | 56 | 46.7 | 64 | 53.3 |
| Mastitis | 59 | 49.2 | 61 | 50.8 |
| Breast abscess | 52 | 43.3 | 68 | 56.7 |
| Leaking milk | 53 | 44.2 | 67 | 55.8 |
| Low milk supply | 55 | 45.8 | 65 | 54.2 |
Table 2. Number and percentage distribution of the studied mothers regarding to lactation barriers of breastfeeding (n=120), total number not mutually exclusive.
Table 3 demonstrated that 62.5% and 80% of the studied mothers agreed that perception of insufficient milk supply and embarrassment from breastfeeding in public places were barriers to breastfeeding respectively.
| Items | Agree | Disagree | ||
|---|---|---|---|---|
| No | % | No | % | |
| Perception of insufficient milk supply | 75 | 62.5 | 45 | 37.5 |
| Postnatal depression | 58 | 48.3 | 62 | 51.7 |
| Embarrassment from breastfeeding in public places | 96 | 80 | 24 | 20 |
| Lack of self-efficacy | 57 | 47.5 | 63 | 52.5 |
| Lack of social support | 56 | 46.7 | 64 | 53.3 |
| Lack of support from father | 58 | 48.3 | 62 | 51.7 |
| Fear of distorted breast shape by breastfeeding | 49 | 40.8 | 71 | 59.2 |
| Unpleasant odor of nursing mother | 50 | 41.7 | 70 | 58.3 |
Table 3. Number and percentage distribution of the studied mothers regarding to psychological barriers to breastfeeding (n=120), total number not mutually exclusive.
Table 4 demonstrated that 74.2% and 59.2% of the studied mothers agreed that caesarean section and twin’s delivery were barriers to breastfeeding respectively.
| Items | Agree | Disagree | ||
|---|---|---|---|---|
| No | % | No | % | |
| Pain following vaginal or caesarean birth | 50 | 41.7 | 70 | 58.3 |
| Caesarean section | 71 | 59.2 | 49 | 40.8 |
| Postpartum fatigue | 44 | 36.7 | 76 | 63.3 |
| New pregnancy | 57 | 47.5 | 63 | 52.5 |
| Twins delivery | 64 | 53.3 | 56 | 46.7 |
| Taking contraceptives | 54 | 45 | 66 | 55 |
Table 4. Number and percentage distribution of the studied mothers regarding to obstetric and gynecological barriers to breastfeeding (n=120).
Table 5 demonstrated that 52.5%, 50.8%, 51.7%, 55%, 53.3% and 50.8% of the studied mothers agreed that post-operative medications, anesthetics and analgesics drugs, antiepileptic’s drugs, immunosuppressant’s, opiates and their derivatives and chemotherapy were barriers to breastfeeding respectively.
| Items | Agree | Disagree | ||
|---|---|---|---|---|
| No | % | No | % | |
| Post-operative medications | 63 | 52.5 | 57 | 47.5 |
| Anesthetics and analgesics drugs | 61 | 50.8 | 59 | 49.1 |
| Antiepileptics drugs | 62 | 51.7 | 58 | 48.3 |
| Immunosuppressants | 66 | 55 | 54 | 45 |
| Opiates and their derivatives | 64 | 53.3 | 56 | 46.7 |
| Chemotherapy | 61 | 50.8 | 59 | 49.1 |
Table 5. Number and percentage distribution of the studied mothers regarding to drug barriers to breastfeeding (n=120), total number not mutually exclusive.
Table 6 demonstrated that 58.3%, 52.5%, 50.8% and 59.2 of the studied mothers agreed that returning to work, promotion and marketing of breast milk substitutes, radiotherapy and breast cancer were barriers to breastfeeding respectively.
| Items | Agree | Disagree | ||
|---|---|---|---|---|
| No | % | No | % | |
| Lack of knowledge about breastfeeding | 54 | 45 | 66 | 55 |
| Returning to work after delivery | 70 | 58.3 | 50 | 41.7 |
| Giving prelacteal feeds | 60 | 50 | 60 | 50 |
| Hospital policies and clinical practices | 49 | 40.8 | 71 | 59.2 |
| Promotion and marketing of breast milk substitutes | 63 | 52.5 | 57 | 47.5 |
| Maternal physical exhaustion | 51 | 42.5 | 69 | 57.5 |
| Lack of personal freedom due to breastfeeding | 48 | 40 | 72 | 60 |
| Radiotherapy | 61 | 50.8 | 61 | 50.8 |
| Breast cancer | 71 | 59.2 | 49 | 40.8 |
Table 6. Number and percentage distribution of the studied mothers regarding to general barriers to breastfeeding (n=120), total number not mutually exclusive.
Table 7 demonstrated that 67.5%, 67.5% and 60% of the studied mothers agreed that cleft lip and cleft palate were barriers to breastfeeding respectively.
| Items | Agree | Disagree | ||
|---|---|---|---|---|
| No | % | No | % | |
| Cleft lip | 81 | 67.5 | 39 | 32.5 |
| Cleft palate | 81 | 67.5 | 39 | 32.5 |
| Tongue tie | 48 | 40 | 72 | 60 |
Table 7. Number and percentage distribution of the studied mothers regarding to infant’s congenital barriers to breastfeeding (n=120), total number not mutually exclusive.
Table 8 demonstrated that 83.3%, 53.3% and 57.5% of the studied mothers agreed that premature infants, poor sucking and swallowing reflexes and breast refusal were barriers to breastfeeding respectively.
| Items | Agree | Disagree | ||
|---|---|---|---|---|
| No | % | No | % | |
| Premature infants | 100 | 83.3 | 20 | 16.7 |
| Down Syndrome | 56 | 46.7 | 64 | 53.3 |
| Breast milk jaundice | 42 | 35 | 78 | 65 |
| Poor sucking and swallowing reflexes | 64 | 53.3 | 56 | 46.7 |
| Insufficient weight gain | 47 | 39.2 | 73 | 60.8 |
| Infant thrush | 44 | 36.7 | 76 | 63.3 |
| Breast refusal | 69 | 57.5 | 51 | 42.5 |
| Poor latch on | 50 | 41.7 | 70 | 58.3 |
Table 8. Number and percentage distribution of the studied mothers regarding to infant’s health barriers hindering breastfeeding (n=120). Total number not mutually exclusive.
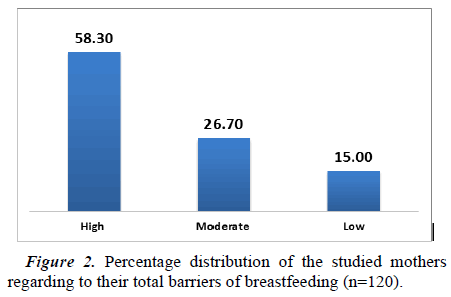
Figure 2 showed that more than half (58.30%) of the studied mothers and their infants had high barriers of breastfeeding. On the other side, 26.7% of them had moderate barriers and 15% had low barriers.
Table 9 described the relation between characteristics of the studied mothers and their total level of knowledge about breastfeeding. There was highly statistically significant relation between mothers knowledge scores and their characteristics including the age, educational level, and numbers of pregnancy (p=0.000, 0.002, and 0.009 respectively). Also, there was statistically significant relation between mothers' knowledge scores and their residence and monthly income (p=0.03 and 0.021 respectively).
| Items | Totalmothers’ knowledge about breastfeeding | χ 2 | p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Good(n=23) | Average(n=39) | Poor(n=58) | |||||||
| No | % | No | % | No | % | ||||
| Age | 20<25 | 1 | 4.3 | 2 | 5.1 | 20 | 34.5 | 21.71 | 0.000** |
| 25<30 | 1 | 4.3 | 26 | 66.7 | 37 | 63.8 | |||
| 30<35 | 8 | 34.9 | 10 | 25.6 | 1 | 1.7 | |||
| 40 ≤40 | 13 | 56.5 | 1 | 2.6 | 0 | 0 | |||
| Educationallevel | Illiterate | 0 | 0 | 0 | 0 | 4 | 6.9 | ||
| Readand write | 0 | 0 | 0 | 0 | 9 | 15.5 | 22.49 | 0.002** | |
| Primary | 0 | 0 | 1 | 2.6 | 7 | 12.1 | |||
| Preparatory | 0 | 0 | 1 | 2.6 | 22 | 37.9 | |||
| Secondary/Technical | 1 | 4.3 | 22 | 56.4 | 16 | 27.6 | |||
| University | 22 | 95.7 | 15 | 38.4 | 0 | 0 | |||
| Residence | Rural | 3 | 13.1 | 18 | 46.2 | 53 | 91.4 | 13.38 | 0.03* |
| Urban | 20 | 86.9 | 21 | 53.8 | 5 | 8.6 | |||
| Occupation | Working | 10 | 43.5 | 16 | 41.1 | 31 | 53.4 | 2.874 | 0.239 |
| Housewife | 13 | 56.5 | 23 | 58.9 | 27 | 46.6 | |||
| Monthlyincome | Enough | 21 | 91.3 | 12 | 30.8 | 3 | 5.2 | 14.78 | 0.021* |
| Notenough | 2 | 8.7 | 27 | 69.2 | 55 | 94.8 | |||
| Numberof pregnancy | 1 | 1 | 4.3 | 5 | 12.8 | 44 | 75.8 | 16.29 | 0.009** |
| 2 | 1 | 4.3 | 13 | 33.3 | 10 | 17.3 | |||
| ≥ 3 | 21 | 91.4 | 21 | 53.9 | 4 | 6.9 | |||
Note: *Significant at p<0.05; **Highly significant at p<0.01; Notsignificant at p>0.05.
Table 9. Relation between characteristics of the studied mothers and their total level of knowledge about breastfeeding (n=120).
Table 10 presented the relation between characteristics of studied mothers and their barriers. There was statistically significant relation between mothers barriers of breastfeeding and their characteristics including the age, educational level, monthly income, and numbers of pregnancy (p=0.040, 0.038, 0.004, 0.002 respectively).
| Items | Totalmothers’ barriers of breastfeeding | χ2 | p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| High(n=70) | Moderate(n=32) | Low(n=18) | |||||||
| No | % | No | % | No | % | ||||
| Age | 20-<25 | 20 | 28.6 | 2 | 6.2 | 1 | 5.6 | 10.51 | 0.040* |
| 25-<30 | 45 | 64.3 | 10 | 31.3 | 9 | 50 | |||
| 30-<35 | 3 | 4.3 | 11 | 34.4 | 5 | 27.8 | |||
| 35 ≤40 | 2 | 2.8 | 9 | 28.1 | 3 | 16.6 | |||
| Educationallevel | Illiterate | 4 | 5.7 | 0 | 0 | 0 | 0 | 7.913 | 0.038* |
| Readand write | 8 | 11.4 | 1 | 3.1 | 0 | 0 | |||
| Primary | 7 | 10 | 1 | 3.1 | 0 | 0 | |||
| Preparatory | 21 | 30 | 1 | 3.1 | 1 | 5.6 | |||
| Secondary/Technical | 26 | 37.2 | 11 | 34.4 | 2 | 11.1 | |||
| University | 4 | 5.7 | 18 | 56.3 | 15 | 83.3 | |||
| Residence | Rural | 42 | 60 | 23 | 71.9 | 9 | 50 | 4.152 | 0.437 |
| Urban | 28 | 40 | 9 | 28.1 | 9 | 50 | |||
| Occupation | Working | 38 | 54.3 | 15 | 46.9 | 4 | 22.2 | 1.344 | 0.742 |
| Housewife | 32 | 45.7 | 17 | 53.1 | 14 | 77.8 | |||
| Monthlyincome | Enough | 5 | 7.1 | 15 | 46.9 | 16 | 88.9 | ||
| Notenough | 65 | 92.9 | 17 | 53.1 | 2 | 11.1 | 17.162 | 0.004** | |
| Numberof pregnancy | 1 | 46 | 65.7 | 2 | 6.2 | 2 | 11.1 | 12.71 | 0.002** |
| 2 | 20 | 28.6 | 3 | 9.4 | 1 | 5.6 | |||
| ≥3 | 4 | 5.7 | 27 | 84.4 | 15 | 83.3 | |||
Note:*Significant at p<0.05; ** Highly significant at p<0.01; Notsignificant at p>0.05.
Table 10. Relation between characteristics of the studied mothers and their total barriers of breastfeeding (n=120).
Discussion
Regarding age of the studied mothers, the current study revealed that more than half of the studied mothers were between 25 and less than 30 years old with ( χ̄ ± SD 27.5 ± 5.98). This result is supported by Hernández-Cordero, et al. [8] study that was conducted in Mexico entitled (Barriers and facilitators to breastfeeding during the immediate and one month postpartum periods, among Mexican women: A mixed methods approach) who reported that the χ̄ ± SD of the studied mothers’ age was 24.16 ± 6.17. From the researcher point of view, this could be due to the similarity in the age of marriage and childbearing in both of the study setting [9-11].
Regarding the level of education, the present study revealed that nearly one third of the studied mothers had secondary/ technical school. This result is supported by Gohal, et al. [7] study that was conducted in Saudi Arabia entitled (Barriers of exclusive breastfeeding among mothers attending primary health care centers in Jazan, Saudi Arabia. descriptive crosssectional study) who found that slightly less than one third of the studied mothers had a secondary education.
Regarding to the total level of knowledge about breastfeeding, the results demonstrated that nearly half of the studied mothers have poor knowledge about breastfeeding. This result is in contrast with Alamirew, et al. [3] study that was conducted in Ethiopia entitled (Knowledge and attitude towards exclusive breast feeding among mothers attending antenatal and immunization clinic at Dabat health center, northwest Ethiopia) who reported that more than two thirds of the studied mothers had good knowledge score about breastfeeding. From researcher point, this result might be due to lack of antenatal or postnatal educational and training programs about breastfeeding in the current study setting.
Regarding to lactation barriers of breastfeeding, the present study revealed that more than three quarters of the studied mothers and more than two thirds of them agreed that sore or cracked nipples and breast engorgement were barriers to breastfeeding respectively. This result is supported by Abdallahb, et al. [1] study that was conducted in Egypt entitled (Breast and nipple problems encountered among puerperal primipara women in Zagazig) who reported that nipple soreness and breast engorgement were the most common problems with highest percentage (85.9% and 82% respectively). From researcher point view, the finding might be due to the improper technique of breast feeding utilized by most of them in addition to lack of experience and support from health care providers in health care settings [12].
Also, the present study revealed that more than half of the studied mothers agreed that pain during breastfeeding was a barrier to breastfeeding. This result is supported by Feenstra, et al. [6] in a study entitled (Early breastfeeding problems: A mixed method study of mothers’ experiences) who stated that early breastfeeding problems frequently occur among Danish mothers 40% were associated with severe pain when breastfeeding.
Regarding to psychological barriers to breastfeeding, the present study showed that most of the studied mothers agreed that embarrassment from breastfeeding in public places was a barrier to breastfeeding. This result is supported by Nguyen, et al. [13] study that entitled (Barriers to exclusive breastfeeding: a cross-sectional study among mothers in ho Chi Minh City, Vietnam) who reported that the top barrier by the perception of the studied mothers was breastfeeding in public place. From researcher point view, the finding might be due to the feelings of shyness, embarrassment and discomfort to expose the breasts because breasts were viewed as sexual objects [14].
Moreover, more than half of the studied mothers agreed that the perception of insufficient milk supply was a barrier to breastfeeding. This result is supported by Abdelnaem, et al. [2] who found that more than half of the mothers reported that the main reason for discontinuing exclusive breastfeeding practice was the perception of insufficient milk supply. From researcher point view, the finding might be due not understanding the normal physiology of lactation which can lead to the perception of an insufficient milk supply when in fact the quantity is enough to nurture the infant.
Regarding to obstetric and gynecological barriers to breastfeeding, the present study revealed that more than half of the studied mothers agreed that caesarean section was a barrier to breastfeeding. This result is supported by Shakya, et al. [15] in a study entitled (Barrier of early initiation of breastfeeding among postnatal mothers) who found that the barrier of early initiation of breastfeeding in more than half of the studied mothers was birth by caesarean section. From researcher point of view, this finding may be due to the lack of practice of initiation of breastfeeding in the recovery room/postoperative room as well as the practice of keeping infants separate from the mother postnatal immediately after caesarean delivery.
Regarding to drug barriers to breastfeeding, more than half of the studied mothers agreed that immune-suppressants were barriers to breastfeeding. From researcher point of view, this finding might be due to the perception that medications cause breast milk to dry up and the perception that some medications can cause harm to the infant if transferred through breast milk.
Regarding to mothers’ general barriers to breastfeeding, the present study showed that more than half of the mothers agreed that returning to the work after delivery was a barrier to breastfeeding. This result is supported by AlKatufi, et al. [4] study that was conducted in Saudi Arabia entitled (Barriers in continuing exclusive breastfeeding among working mothers in primary health care in the ministry of health in Al-Ahsa region, Saudi Arabia) who reported that early returning to the work was a barrier to exclusive breastfeeding in more than two thirds of the studied mothers. From researcher point view, the finding might be due to lack of knowledge about expressing breast milk as an alternative way for breastfeeding during work hours and the lack of enough time and absence of worksite private places to pump during the work hours [16].
Regarding infants’ health barriers to breastfeeding, the present study revealed that more than half of the studied mothers agreed that breast refusal was a barrier to breastfeeding. Also, this result is supported by Abdallahb, et al. [1] who stated that more than two fifths of mothers reported that infant refusal of breast milk as a difficulty encountered among breastfeeding mothers.
Moreover, the present study revealed that most of the studied mothers agreed that prematurity was a barrier to breastfeeding. This result is in contrast with Gohal, et al. who found that only ten percent of the studied mothers agreed that premature birth and the inability of the baby to breastfeed was a barrier to breastfeeding.
Regarding total barriers of breastfeeding, the present study showed that more than half of studied mothers and their infants have high barriers of breastfeeding. On the other side, more than one quarter of them have moderate barriers and few of them have low barriers. This finding is in contrast with Gohal, et al. [7] who reported most of the studied mothers are not agree with most of the barriers of breastfeeding. From the researcher point of view, this finding might be due to low level of education, their information about breast feeding obtained from their relatives and friends not from scientific source and lack of antenatal counseling about breastfeeding.
Regarding to the relationship between mothers' total level of knowledge about breastfeeding and their characteristics. The present study revealed that there was highly statistically significant relationship between mothers' total knowledge scores and their characteristics including the age, educational level, and numbers of pregnancy (p=0.000, 0.002, and 0.009 respectively). Also, there was statistically significant relationship between mothers' knowledge scores and their residence and monthly income (p=0.03 and 0.021) respectively.
This outcome goes in the same line with Kareem, et al. [10] who conducted study about (Effectiveness of teaching program on knowledge regarding the breastfeeding problems among postnatal mothers) and showed that there was highly statistically significance different between the mothers’ characteristics such as occupation, education, and income with studied mothers’ level of knowledge.
Regarding to the relation between characteristics of mothers and their total barriers of breastfeeding. The present study revealed that there was statistically significant relationship between mothers’ total barriers of breastfeeding and some of their characteristics including the age, educational level, monthly income, and numbers of pregnancy (p=0.040, 0.038, 0.004, 0.002 and respectively). This finding is supported by Kandeel, et al. [9] study that was conducted in Egypt entitled (Determinants of exclusive breastfeeding in a sample of Egyptian infants) who found that there was statistically significant relationship between mothers’ barriers of breastfeeding and their characteristics including the age and numbers of pregnancy (p<0.001) [17].
Conclusion
The findings of this study were concluded that the most common barriers of breastfeeding related to mothers were pain during breastfeeding, sore or cracked nipples, breast engorgement, perception of insufficient milk supply, embarrassment from breastfeeding in public places, cesarean section, immunosuppressant’s, returning to work after delivery and breast cancer. Meanwhile the most common barriers related to infants were cleft lip, cleft palate, premature infants and breast refusal. Also, there was statistically significant relationship between mothers’ barriers of breastfeeding and some of their characteristics including the age, educational level, monthly income and numbers of pregnancy.
Ethical Considerations
The research approval was obtained from the faculty of nursing of Helwan university ethical scientific research committee before starting the study. The researcher was clarified the objectives and aim of the study to mothers included in the study before starting. Verbal approval was obtained from the mothers before inclusion in the study; a clear and simple explanation was given according to their level of understanding. They secured that all the gathered data was confidential and used for research purpose only. The researcher was assuring maintaining anonymity and confidentiality of subjects' data included in the study. The mothers were informed that they can choose to participate or not in the study and they have the right to withdrawal from the study at any time.
Recommendations
In the light of the findings of the current study the following recommendations are suggested:
• Early detection and adequate management of barriers hindering breastfeeding of infants in the first year of life.
• Increasing mothers’ knowledge about barriers of breastfeeding and how to overcome them through frequent educational programs.
• Educating and providing psychological support for newly mothers about importance of early inanition of breastfeeding and exclusive breastfeeding at health care settings.
• Further research about barriers of breastfeeding with increasing sample size in different health care settings.
Research questions
• What are the barriers of breastfeeding in the first year of life?
• Is there a relationship between barriers of breastfeeding and mothers' characteristics?