Current Pediatric Research
International Journal of Pediatrics
Assessment of umbilical venous catheter insertion depth using Dunn and Shukla method.
Ali Adel Shareef1*, Ruaa F Mohammed1, NazarAbdulkadir Kandla2
1 Department of Pediatrics, College of Medicine, Ninevah University, Mosul, Iraq
2 Department of Pediatrics, College of Medicine, University of Mosul, Mosul, Iraq
- Corresponding Author:
- Ali Adel Shareef
Department of Pediatrics
College of Medicine
Ninevah University
Mosul
Iraq
Tel: +964 771-291-3336
E-mail: aliael@uoninevah.edu.iq
Accepted date: 15th September, 2021
Objectives: Umbilical venous catheterization is a commonly used intervention in the Neonatal Intensive Care Unit (NICU), and it is important to estimate the optimal depth of catheter insertion in order to minimize complications of catheterization. The aim of this study was to compare Dunn and Shukla's methods for predicting the length of umbilical venous catheter insertion at varying birth weight. Materials and Methods: This is a prospective comparative study conducted on newborns subjected to Umbilical Venous Catheterization (UVC) at the NICU at AL-Khansaamaternity and children’s teaching hospital, Mosul, Iraq over 12 months beginning on 1 August 2019. The catheter tip position was evaluated with thoracoabdominal AP radiographs and considered correct if the tip was visible between T9 and T10, under insertion (below T10), and over-insertion (above T9). Results: A total of 111 infants were enrolled during the study period. Fourteen infants were excluded because their UVCs tips were located laterally in the portal venous system and the remaining 97 infants were analyzed, of which 49 were allocated to Dunn’s group and 48 to Shukla’s group randomly.Dunn's method was more accurate than Shukla’s method for determining the optimal insertion length of UVCs (45% vs. 25%, P=0.04); especially in infants with birth weight <1500 g (59% vs. 11%, P=0.00296). Whereas, a significantly higher rate of highly positioned catheter tips was demonstrated in Shukla's method than in Dunn's method (73% vs. 51%, P=0.0264); and especially in infants with birth weight <1500 g (89% vs. 35%, P=0.00104). While the analysis did notshow any significant difference in the proportions of low positioned catheter tips between the two groups. Conclusion: This study showed that Dunn’s method resulted in a higher rate of ideal insertion length of UVCs than Shukla’s method. The rate of correctly positioned catheter tip was significantly high in Dunn’s method especially in infants with birth weight <1500 g. whereas, the rate of highly positioned catheter tip was significantly high in Shukla’s method particularly in infants with birth weight <1500 g.
Keywords
Umbilical venous catheter, Dunn method, Shukla method.
Introduction
Umbilical vein catheterization is a widely used procedure in neonatal intensive care units, which provides immediate vascular access for newborns, especially those who are preterm or have severe morbidity shortly after birth [1]. It provides reliable intravenous access for blood sampling, monitoring of central venous pressure, exchange transfusions and administration of parenteral nutrition, medications, and blood products [2,3]. In spite of the benefits and implementations of the umbilical vein catheterization, its possible complications must also be taken into consideration. Many of these serious complications, such as pericardial effusions, cardiac tamponade, arrhythmia, endocarditis, intracardiac thrombosis, liver hematoma, and portal vein thrombosis, are directly related to Umbilical Vein Catheter (UVC) insertion in an inappropriate location [4-6]. The ideal location of the UVC tip to minimize complications should be outside the heart at the junction of Inferior Vena Cava (IVC) with the Right Atrium (RA) [7,8].
Several methods and formulae have been described for estimating the appropriate insertion depth for UVC [9]. The two methods which are most commonly used are Dunn and Shukla [10,11]. The principle of the Dunn method is based on plotting the shoulder-umbilicus length on a special graph relating this measurement to the estimated insertion depth for UVC [10]; whereas the Shukla method uses an equation based on birth weight of the neonates [11]. The location of the catheter tip must be verified radiologically, thoracoabdominal AP radiographs being the most commonly used technique[12,13]. On radiographs, the ideal location of the UVC tip usually corresponds to the ninth or tenth thoracic vertebrae (T9-T10), at or slightly above the diaphragm[14,15]. However, bedside ultrasound and echocardiogram are increasingly used for this purpose [16,17].To the best of our knowledge, no prospective study has compared Dunn’s method with Shukla’s formula in Iraq.Given the serious complications of improperly located UVCs. Therefore, this study aimed to compare the efficacy of Dunn and Shukla methods in predicting the ideal UVC insertion depth, as assessed by AP thoracoabdominal radiographs and the impact of birth weight on proper catheter insertion.
Materials and Methods
This prospective comparative study was conducted at the NICU at Al-Khansaamaternity and children's teaching hospital, Mosul, Iraq, from 1 August 2019 to 31 July 2020. The study protocol was approved by the ethics committee at Ninevah medical college.
Figure 1: Shoulder-umbilicus length ,which is the vertical distance from the top of the shoulder at the lateral clavicle end to an imaginary horizontal line passing through the center of umbilicus as described by Dunn [10].
Neonates, who needed UVC insertion for exchange transfusion, hyperosmolar solution and blood products infusion, and those with multiple failed peripheral intravenous access, were eligible for enrollment in this study. While those with omphalitis, omphalocele, gastroschisis, hydropsfetalis, peritonitis, necrotizing enterocolitis, congenital diaphragm hernia, major structural cardiac disease, and those in whom catheters were mistakenly inserted in the umbilical artery or in the portal venous system, were excluded from the study. The decision to insert umbilical catheters was made by the attending physician. UVCs were inserted according to local clinical guidelines under sterile conditions.
A total of 111 newborns were assigned either to Dunn's method or Shukla's formula groups according to the pre-insertion calculation of the UVC insertion depth. In the Dunn group, we calculated the insertion depth by measuring the vertical distance from the infant's shoulder tip to the level of the center of the umbilicus (Figure1), and then we plotted this measurement on the Dunn nomogram [10]. While in the Shukla group, the insertion depth estimated using a formula described by Shukla and Ferrara [11], which is a body weight-based equation: UVC insertion length=(birth weight × 3+9)/2+1.
Electronic weight scale was used to measure the weight of all infants admitted to the NICU. We have pushed the catheters until the marker showing the estimated insertion depth is at the level of the skin on the abdominal wall. Radio-opaque polyurethane UVCs, 3.5 Fr and 5.0 Fr were used to catheterize neonates <1500 g and ≥ 1500 g, respectively. The position of the UVC tip was verified by the supine AP thoracoabdominal radiograph, the radiographer and the radiologist who assessed the position of the catheter tip were masked for group assignments. We used the radiographs to confirm the position of the catheter tip and to relocate it correctly.
The radiography also helped in determining the outcome of this study. Correct position of the UVC was described as the catheter tip being visible between T9 and T10 on radiography, at or slightly above the diaphragm [18]. The position of the UVC tip was considered to be in high position if the tip of the catheter was above the upper border of T9, and in low position if the tip was below the lower border of T10. No consent was required from the parents, as this is a standard procedure carried out following the general admission consent and the NICU clinical guidelines, and written informed consent was obtained for the enrollment in the study. Neonate’s gestational age, gender, birth weight, and mode of delivery were recorded. Subjects were divided into subgroups based on birth weight (<1500 g and ≥ 1500 g) and gestational age (<37 weeks and ≥ 37 weeks).
Infants were randomly assigned to either Dunn or Shukla groups in a 1:1 ratio. The randomization was concealed from the treating healthcare providers and was strati?ed by birth weight (<1500 g or ≥ 1500 g) and gestational age (<37 weeks and ≥ 37 weeks).The group assignments were printed on cards that were folded and placed in sequentially numbered, sealed, opaque envelopes. The envelopes were opened just before UVC insertion was attempted in the NICU.
Statistics
Data were collected using Microsoft excel 2013 and statistical analysis was performed using IBM SPSS statistics version 20. Categorical variables were compared using chi-square test or fisher’s exact test as appropriate. Normally distributed continuous variables were compared by two-sample unpaired t-test (the student's t-test), whereas Mann–Whitney test was used to compare not normally distributed values. AP<0.05 was considered statistically significant.
Results
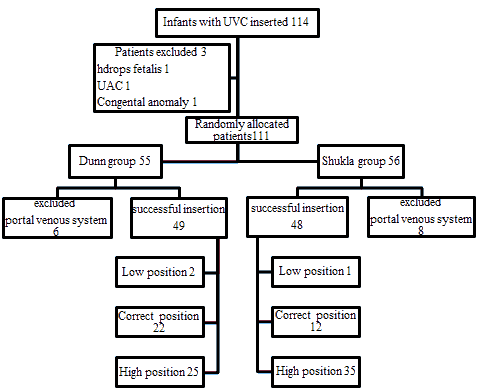
There were 114 infants admitted to our NICU during the 12 month study period who were subjected to an attempted UVC insertion. Three infants were not enrolled in the study, and 111 infants were allocated randomly to 55 for Dunn’s group and 56 for Shukla’s group. Fourteen of the 111 allocated infants were later excluded from the analysis because their UVCs tips were located laterally in the portal venous system and the data from 97 infants were analyzed, of which 49 were allocated to Dunn's group and 48 to Shukla'sgroup (Figure 2).
In terms of demographic characteristics including gender, birth weight, gestational age and mode of delivery, no statistically significant differences were observed between the two groups (p>0.05) (Table 1).
| Dunn group(n=49) | Shukla group(n=48) | P | |
|---|---|---|---|
| Gender | |||
| Male (n(%)) | 26 (53%) | 23(48%) | 0.612 |
| Female (n(%)) | 23(47%) | 25(52%) | |
| Birth weight (g)Median (IQR) | 1800(1300-3000) | 1950(1312-3000) | 0.894 |
| ≥ 1500 g (n(%)) | 32(65 %) | 30(62.5 %) | |
| <1500 g (n(%)) | 17(35 %) | 18(37.5 %) | |
| Gestational age (weeks)Median (IQR) | 34(32-38) | 34(32-37) | 0.793 |
| ≥ 37weeks (n(%)) | 15(31%) | 13(27%) | |
| <37weeks (n(%)) | 34(69%) | 35(73%) | |
| Mode of delivery | |||
| C/S (n(%)) | 9(18%) | 11(23%) | 0.580 |
| NVD (n(%)) | 40(82%) | 37(77%) |
Table 1. Demographic profile of the patients. C/S: Cesarean Section; NVD: Normal Vaginal Delivery.
Comparison of positions of the umbilical venous catheter tip between Dunn and Shukla groups revealed a significantly higher rate of correctly positioned catheter tips in Dunn's group 45% (22/49) as compared with 25% (12/48) in Shukla's group (P=0.04). Whereas, significantly high rate of highly positioned catheter tip were found in Shukla's group 73 % (35/48) against 51% (25/49) in Dunn's group (p=0.0264). Furthermore, Fisher’s exact testdid not show a significant difference between Dunn's group 4% (2/49) and Shukla's group 2% (1/48) with respect to the low positioned UVCs tips (p=1.0) (Table 2).
| Dunn group | Shukla group | P | |
|---|---|---|---|
| Catheter position | n(%) | n(%) | |
| Low position | 2 (4%) | 1(2%) | 1.0 |
| Correct position | 22(45%) | 12(25%) | 0.0400 |
| High position | 25(51%) | 35(73%) | 0.0264 |
| Total | 49 | 48 |
Table 2. Comparison of umbilical venous catheter tip position in Dunn and Shukla groups as determined by radiograph.
In order to ascertain the impact of birth weight on the proper insertion of the catheter, further analysis was conducted to compare the level of the catheter tip between the Dunn and Shukla groups with a birth weight <1500 g and ≥ 1500 g. In infants with birth weight <1500 g, there was a significantly higher proportion of correctly placed UVCs in Dunn's group 59% (10/17) vs. Shukla's group 11% (2/18) (p=.00296). Whereas, the rate of highly positioned catheter tips in Shukla's group 89% (16/18) was significantly high compared to that in Dunn's group 35% (6/17) (p=.00104). While, the analysis did not show any significant difference in the proportions of low positioned catheter tips between the two groups, Dunn 5.8% ( 1/17) vs. Shukla 0% (0/18) (p=.485) (Table 3).
| Catheter position | Bwt <1500 g | P | Bwt ≥ 1500 g | P | ||
|---|---|---|---|---|---|---|
| Dunn group | Shukla group | Dunn group | Shukla group | |||
| Low position | 1 (5.8% ) | 0 (0%) | 0.485 | 1 (3% ) | 1 (3% ) | 0.963 |
| Correct position | 10 (59% ) | 2 (11%) | 0.00296 | 12 (38% ) | 10 (34%) | 0.732 |
| High position | 6 (35% ) | 16 (89%) | 0.00104 | 19 (59% ) | 19 (63%) | 0.749 |
| Total | 17 | 18 | 32 | 30 | ||
Table 3. Comparison of the position of the umbilical venous catheter tip in birth weights <1500 g and ≥ 1500 g in the Dunn and Shukla groups, as determined by radiograph.
In infants with birth weight ≥ 1500 g, the analysis did not reveal any significant difference in the rate of correctly positioned UVCs tips between Dunn's group 38% (12/32) and Shukla's group 34% (10/30) (p=.732). Similarly, in comparing the rate of highly positioned UVCs tips in Dunn 59% (19/32) and Shukla groups 63% (19/30), the Chi-square test did not show a statistically significant difference (p=.749). Also, in terms of low positioned UVCs tips, there was no significant difference between Dunn's group 3% (1/32) and Shukla's group 3% (1/30) (p=.963) (Table 3).
Discussion
Umbilical vein catheterization is one of the essential procedures in the neonatal units, yet it carries a lot of complications [19]. Many of these complications are directly related to malpositioning of the catheter tips, either high or low [20]. In the present study, we compared two of the most widely used methods in calculating the ideal site of catheter tip. The Dunn's method, which uses surface measurement, plotted on special nomogram, and the Shukla formula, which depends on infant's body weight. The position of the UVC tip has been verified radiologically by supine AP thoracoabdominal radiograph.
In the present study, the rate of correctly positioned catheter tips in Dunn's group was significantly high (45%) compared to (25%) in Shukla's group (P=0.04). Whereas, the rate of highly positioned catheter tips in Dunn's group was significantly low (51%) in comparison to that in Shukla's group (73%) (p=0.00295). No significant difference in the proportions of low positioned catheter tips between the two groups was observed. These results seem to be consistent with a study conducted in the Netherlands in 2010 by Verheij et al. who reported a higher rate of correctly positioned UVC tips by using the Dunn’s nomogram (41%), compared with Shukla’s formula (24%). Similar to our study, Verheij et al. reported a significantly high rate of UVC tips being placed at high positions in Shukla's method (75%) against (51%) in Dunn's group, and in terms of low positioned catheter tips, they also reported no significant difference between the two groups. In another study conducted by Verheij et al. a higher rate of highly positioned UVC tips was consistently observed in Shukla's group (73%), and the UVC was directly placed incorrect position in (26%), findings which are comparable to our study [15,21].
Kieran et al. conducted a randomized controlled trial in Ireland, compared Dunn’s method and Shukla’s formula and observed no difference in the rate of correctly positioned UVC tips between Dunn (28%) and Shukla (31%) methods[14]. The rate of correct catheter insertion using Dunn's method in this study was far below that observed in our study (45%). This discrepancy could be attributed to the high inconsistency in the measurement of shoulder to umbilicus distance by different pediatric professionals, which is used in Dunn's method. In the Netherlands, Lopriore et al. interviewed 101 pediatric professionals and reported that only 14% of them selected the proper technique for measuring this distance, which is the vertical distance from the top of the shoulder at the lateral clavicle end to an imaginary horizontal line passing through the center of umbilicus at the level of abdomen (Figure 1) [22].
In our study, the rate of correctly positioned UVC tips in infants with birth weight <1500 g in Dunn's group (59%) was significantly higher than Shukla's group (11%). Whereas, the rate of high positioned catheter tips was significantly higher in Shukla's group (89%) vs. (35%) in Dunn's group. Gupta et al. conducted in 2015 and observational study compared Shukla's formula with other four morphometric measurements at varying birth weights and reported that in infants with birth weights ≤ 1500 g, Shukla's formula resulted in (46%) correctly positioned UVC tips which is significantly higher than that observed in our study and (49%) catheter tips that positioned at high levels, a result which is significantly lower than the present study [23]. Our results do not appear to corroborate their observation, in fact, small sample size in our study might account for this discrepancy, other possible explanation, is that the design of Gupta’s study was not prospective. Shetaet al. conducted a randomized controlled trial in Canada compared Shukla’s formula with a Surface Measurement (SM) based on umbilicus to nipple distance and observed that among ELBW infants, more infants assigned to SM method had correctly positioned UVC tip as compared with Shukla’s formula (43.7% vs. 22.5%), which is in line with our study [24]. Goodarzi et al. carried out an observational study comparing Dunn's method and Shukla's formula and reported that Shukla's formula resulted in a higher rate of appropriately inserted UVC than Dunn's method (59.5% vs. 42%)in infants with birth weight <1500 g [25]. This result is in contrast to our study; a possible explanation for this might be that, in contrast to the mentioned study, we had excluded from the study all cases where the tips of UVCs were located in the portal venous system.
Our study did not reveal any significant differences in rates of correct positioned, high positioned, and low positioned UVC tips between Dunn's method and Shukla's formula in those infants with birth weight ≥ 1500 g. Our results are in agreement with that of Goodarzi's study 25, but differ from the results of Gupta's study [23], who reported a higher rate of correctly positioned UVC tips (64%), and lower rate of highly positioned UVC tips (28%) than our study, when Shukla’s formula was used. The contradictory findings may be explained by the greater sample size in Gupta's study, and the higher median birth weight 2000 g (490–4800).
The most obvious limitation of this study was the relatively small sample size. Second, as per unite policy, the location of the catheter tips was only verified by AP radiographs to minimize radiation exposure. However, as the proximal part of the ductus venosus runs in the anteroposterior plane before joining the IVC, therefore, it cannot be visualized by AP view [26]. In addition, it may be difficult to determine the catheter tip as it projects over the vertebrae in AP view. Lateral radiographs, in addition to the AP view, are therefore required to overcome these flaws [27,28]. Finally, the research findings of this study were limited by the inability to use echocardiography or real-time ultrasonography, as a more reliable method to verify more precisely the exact level of UVC tip as advocated by many authors [29,30]. The strengths of our study are the good homogeneity and comparability of the two study groups in terms of birth weight and gestational age. In addition, the radiographs were read by a single radiologist who was masked to the group assignment.
Conclusion
According to the findings of the current study, it is evident that the efficacy of Dunn and Shukla methods in estimating the ideal insertion depth of UVC was unsatisfactory. Shukla’s formula resulted in significantly higher rate of highly positioned catheter tip particularly in infants with birth weight <1500 g. While the rate of correctly positioned catheter was significantly higher in Dunn's method especially in infant with birth weight <1500 g.
Infants with UVC located laterally in the portal system were excluded early from this study; therefore, the rate of low-lying UVC tip in both groups was not significant. Catheters inserted at an inappropriately high position, were more practically re-adjusted by pulling them if the sterile field was not disrupted, while catheters in low positions had to be replaced and the procedure recommenced again.
Further researches with larger sample size are suggested to derive more reliable and accurate formulae, which depend on fixed anatomical landmarks to predict the optimal UVC insertion depth. The use of echocardiography or real-time ultrasonography is highly recommended since it provides a more reliable assessment of the level of UVC tip, otherwise, in addition to the AP view; lateral radiographs should be standard to enhance verification of the level of UVC tips.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Interest
The authors have no conflicts of interest to disclose.
Acknowledgements
The authors would like to thank the pediatric senior house officers and the nurses who assisted in patient's recruitment.
References
- Khasawneh W, Samara DN, Bataineh ZA. Umbilical catheter rupture: A serious complication in neonatal intensive care units. Int. J Pediatr Adolesc Med 2020; pp: 146-148.
- Michaels A, Wolf JM, Gomella TL, et al. Venous access: Umbilical vein catheterization.Gomella's Neonatology. (8th edn). New York: McGraw-Hill 2020; pp: 417-423.
- Mutlu M, Kucukalioglu PB, Aslan Y, et al. Comparison of methods and formulas used in umbilical venous catheter placement. Turk Pediatri Ar?ivi 2017; 52(1): 35-42.
- Michel F, Brevaut-Malaty V, Pasquali R, et al. Comparison of ultrasound and X-ray in determining the position of umbilical venous catheters. Resuscitation 2012; 83(6): 705-9.
- Stuttaford L, Webb J, Smith SL, et al. Estimating insertion length of umbilical arterial and venous catheters in newborn infants: time for change. J Matern Fetal Neonatal Med 2020; pp: 1-6.
- Franta J, Harabor A, Soraisham A. Ultrasound assessment of umbilical venous catheter migration in preterm infants: a prospective study. Arch Dis Child Fetal Neonatal Ed 2017; 102(3): 251-255.
- Harabor A, Soraisham A. Rates of intracardiac umbilical venous catheter placement in neonates. J Ultrasound Med 2014; 33(9): 1557-1561.
- Finn D, Kinoshita H, Livingstone V, Dempsey E. Optimal line and tube placement in very preterm neonates: an audit of practice. Children 2017; 4(11): 99.
- Deshabhotla S, Vallala V, Tandur B, et al. Comparison of Dunn and Shukla method of calculating umbilical vein catheter insertion length: A randomized controlled trial. J Neonatal Nurs 2019; 25(5): 249-253.
- Dunn PM. Localization of the umbilical catheter by post-mortem measurement. Arch Dis Child 1966; 41(215): 69-75.
- Shukla H, Ferrara A. Rapid estimation of insertional length of umbilical catheters in newborns. Am JDis Child 1986; 140(8): 786-788.
- Simanovsky N, Ofek-Shlomai N, Rozovsky K, et al. Umbilical venous catheter position: evaluation by ultrasound. Eurradiol 2011; 21(9): 1882-1886.
- Krishnegowda S, Thandaveshwar D, Mahadevaswamy M, et al. Comparison of JSS formula with modified Shukla’s formula for insertion of umbilical venous catheter: A randomized controlled study. Indian Pediatr 2019; 56(3): 199-201.
- Kieran E, Laffan E, O'Donnell C. Estimating umbilical catheter insertion depth in newborns using weight or body measurement: a randomised trial. Arch Dis Child Fetal Neonatal Ed 2016; 101(1): 10-15.
- Verheij G, te Pas A, Witlox R, et al. Poor accuracy of methods currently used to determine umbilical catheter insertion length. Int J Pediatr 2010.
- El-Maadawy SM, El-Atawi KM, Elhalik MS. Role of bedside ultrasound in determining the position of umbilical venous catheters. J Clin Neonatol 2015; 4(3): 173.
- Karber BC, Nielsen JC, Balsam D, et al. Optimal radiologic position of an umbilical venous catheter tip as determined by echocardiography in very low birth weight newborns. J Neonatal Perinatal Med 2017; 10(1): 55-61.
- Michael HWG. Comparing two formulas to estimate the correct depth of the neonatal umbilical venous catheter insertion. J Med Sci Res 2019; 2(2): 137-143.
- Mutlu M, Aslan Y, Kul S, et al. Umbilical venous catheter complications in newborns: a 6-year single-center experience. The J Matern-Fetal Neonatal Med 2016; 29(17): 2817-2822.
- Hoellering AB, Koorts PJ, Cartwright DW, et al. Determination of umbilical venous catheter tip position with radiograph. Pediatr Crit Care Med 2014; 15(1): 56-61.
- Verheij G, Te Pas A, Smits-Wintjens V, et al. Revised formula to determine the insertion length of umbilical vein catheters. Eur J Pediatr 2013; 172(8): 1011-1015.
- Lopriore E, Verheij G, Walther F. Measurement of the ‘Shoulder-Umbilical’ distance for insertion of umbilical catheters in newborn babies: Questionnaire study. Neonatology 2008; 94(1): 35-37.
- Gupta AO, Peesay MR, Ramasethu J. Simple measurements to place umbilical catheters using surface anatomy. J Perinatol 2015; 35(7): 476-480.
- Sheta A, Soraisham A, Kamaluddeen M. Umbilical venous catheter insertion depth estimation using birth weight versus surface measurement formula: a randomized controlled trial. J Perinatol 2019; 40(4): 567-72.
- Goodarzi R, Tariverdi M, Barchinejad M, et al. Dunn method suitability in umbilical catheter length prediction on Newborns compared to Shukla. Asian J Med Pharm Res. 2014; 4(2): 85-90.
- Guimarães AF, De Souza AA, Bouzada MC, et al. Accuracy of chest radiography for positioning of the umbilical venous catheter. J Pediatr 2017; 93(2): 172-178.
- Lean WL, Dawson JA, Davis PG, et al. Accuracy of five formulae to determine the insertion length of umbilical venous catheters. Arch Dis Child Fetal Neonatal Ed 2019; 104(2): 165-9.
- Butler G, Al-Assaf N, Tarrant A, et al. Using lateral radiographs to determine umbilical venous catheter tip position in neonates. Ir Med J 2014; 107(8): 256-258.
- Ades A, Sable C, Cummings S, et al. Echocardiographic evaluation of umbilical venous catheter placement. J Perinatol 2003; 23(1): 24-28.
- Sharma D, Farahbakhsh N, Tabatabaii SA. Role of ultrasound for central catheter tip localization in neonates: a review of the current evidence. J Matern Fetal Neonatal Med 2019; 32(14): 2429-2437.