Current Pediatric Research
International Journal of Pediatrics
Age affects lateral spurring after pediatric humerus lateral condyle fractures: A retrospective cohort study.
Tao Liu1, Chuan Dong2, Wu Wen3, Nan Li3*
1Department of Orthopedics, General Hospital of Xinjiang military command, Urumqi 830099, Xinjiang Uygur Autonomous Region, China
2Department of Orthopedics, Tangdu Hospital, Air Force Medical University, Xi’an 710032, Shanxi, China
3Department of Orthopedics, 96603 Military Hospital of PLA, Huaihua 418000, Hunan, China
- Corresponding Author:
- Nan Li
Department of Orthopedics, 96603 Military Hospital of PLA, 65 Huaidong Road, Huaihua 418000, China
E-mail: 958695747@qq.com
Received: 25 September, 2023, Manuscript No. AAJCP-23-120598; Editor assigned: 27 September, 2023, Pre QC No. AAJCP-23-120598 (PQ); Reviewed: 11 October, 2023, QC No. AAJCP-23-120598; Revised: 18 October, 2023, Manuscript No. AAJCP-23-120598 (R); Published: 25 October, 2023, DOI:10.35841/0971-9032.27.07.2002-2008.
Background: Lateral spurring is frequently observed after lateral condyle fractures of the humerus in children. Despite its frequent recognition, few previous studies have defined this phenomenon, explored a correlation with any fracture or treatment characteristics, nor assessed its clinical significance.
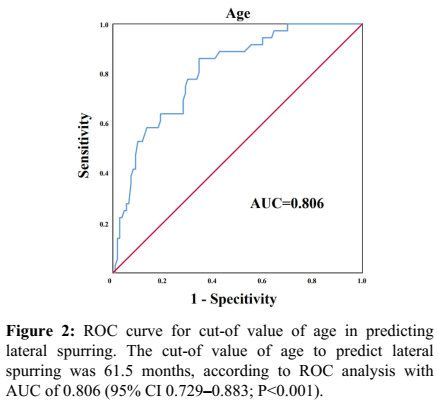
Methods: Information of 146 lateral condyle fractures in children from June 2015 to September 2021 were retrospectively analyzed and a database was established. Lateral spurring was defined as a bony overgrowth over the lateral aspect of the lateral condyle resulting in imaging irregularity on radiography. Univariable and multivariable logistic regression analyses were used to identify independent risk factors for lateral spurring, and a Receiver Operating Characteristic (ROC) curve was used to assess the impact of independent risk factors.
Results: Among the 146 fractures identified, 6.6% were treated with cast immobilization, 93.4% with open reduction and internal fixation, and none with closed reduction and percutaneous pinning. In total, 110 (75.3%) patients developed a lateral spur, age was identified as an independent risk factor for lateral spurring (P<0.001), and the Area Under the ROC Curve (AUC) was 0.806(95% Confidence Interval (CI) 0.729-0.883, P<0.001). At age 61.5 months, the Youden index reached its maximum with a sensitivity of 86.1% and specificity of 65.5%, Patients with age less than 61.5 months had a higher lateral spurring, the Relative Prevalence (RP) was 1.70.
Conclusions: The development of lateral spurring closely correlates with patient age, the incidence of lateral spurring decreases with age, the incidence of lateral spurring was higher in patients younger than 61.5 months. The presence of a lateral spur after an LCF of the humerus does not influence the function or the appearance of the elbow.
Level of Evidence: Level ?— retrospective study.
Keywords
Lateral, Condyle, Fracture, Spur, Pediatric
Introduction
Lateral Condyle Fractures (LCFs) are the second most common pediatric fractures and comprise 12%-20% of all pediatric upper extremity fractures [1]. These fractures most commonly occur in children 4 to 10 years of age, with the highest incidence in children 6 years of age, and have been widely concerned because of their complicated complications [2]. Non displaced pediatric LCFs are often treated with cast immobilization; however, displaced fractures often need surgical treatment to reduce the incidence of complications, such as nonunion, deformity, and arthritis [3,4]. Depending on the classification and the amount of displacement of pediatric LCFs, Closed Reduction with Percutaneous Pinning (CRPP) or Open Reduction with Internal Fixation (ORIF) will be applied.
The outcome of pediatric LCFs has been extensively discussed in the literature [5,6]. However, as the most common complication of LCFs, a “lateral spur”, has seldom been investigated [2,7,8], it has been described as a bony overgrowth over the lateral of the distal humerus after the healing of pediatric LCFs. The formation of the lateral spur often occurs as the result of bone healing, about 2-6 weeks after the fracture [9]. A “lateral spur” is not only a radiographic phenomenon, but also a clinical finding as well, as it is often palpable and thus frequently noted by patients, parents and physicians, inducing wide concern [2,10].
Our study aimed to identify the potential risk factors for lateral spurring by analyzing data that have been collected retrospectively as part of an ongoing Institutional Review Board-approved data-collection project on pediatric elbow fractures. If the risk factors can be identified, their influence to the occurrence of lateral spurring will be assessed by statistical analysis. Moreover, whether lateral spurring has an effect to the appearance or function of the elbow will be clarified. By probing into lateral spurring, we aim to better the phenomenon of lateral spurring and provide information for physicians to better educate patients and families.
Materials and Methods
Patient selection
From June 2015 to September 2021, the clinical data of LCFs patients younger than 15 years of age admitted to our hospital were collected and a database was established as part of an Institutional Review Board-approved study on pediatric elbow fractures. The patient’s inclusion was based on radiographic diagnosis. All elbows were evaluated with standard AP and lateral radiographs, performed by experienced technicians and uploaded into our digital radiology package (INFINITT PACS V 3.0.10.2 BN3 20100614; INFINITT Healthcare Co., Ltd). All radiographs were taken at a fixed distance of 3.61 inches using the same digital x-ray machine (Digital Diagnost DiDi Eleva01 2.1.4v22.13.567, PHILIPS).
Parameter selection
The clinical characteristics of all patients were obtained from their medical records. The characteristics of interest included age, sex, Body Mass Index (BMI), side of injury, initial displacement, type of treatment, type of fracture, delayed fracture (injury >2 weeks) or not, combined with other elbow injury or not, the Mayo Elbow Performance Score (MEPS), Range Of Motion (ROM) loss, and complications. Fracture initial displacement <2 mm, between 2-4 mm and >4 mm. All of the fractures were Milch type 2, so only Jacob fracture type were adopted [11,5]. ROM loss was divided into 4 degrees: <15°C ROM loss was defined as mild elbow mobility disorder, 15°C-30°C ROM loss was moderate, 30°C-50°C ROM loss was severe, and >50°C ROM loss was extremely. MEPS were divided into 4 categories: A score >90 was defined as excellent, 75-89 as good, 60-74 as medium, and <60 as poor. Complications included cubitus varus, cubitus valgus, nonunion, fishtail deformity, avascular necrosis, incision infection, and subjective lateral prominence. By measuring the elbow carrying angle in the Anteroposterior (AP) radiograph, carrying angles less than -5°C or greater than 15°C were defined as cubitus varus or cubitus valgus, respectively. Information on subjective lateral prominence was obtained by telephone follow-up, and the patient's parents were asked whether a lateral prominence could be seen by general appearance.
Treatment method
The type of treatment was decided by the fractures’ initial displacement [9]. The greatest distance between the two fragments on any single view of AP and lateral radiograph was measured and documented as the initial displacement. Conservative treatment with long-arm immobilization was used for fractures displaced by <2 mm. A closed reduction under anesthesia was attempted for fractures displaced between 2-4 mm. For fractures with an initial displacement >4 mm and for those >2 mm after closed reduction, ORIF was performed. All surgeries were performed by experienced surgeons using a standard lateral approach incision. Two Kirschner wires (1.5 mm diameter) were used for the fixation of fresh fractures, and a metal hollow screw (3.5 mm diameter) and a Kirschner wire were used for delayed fractures. All operative fractures used an ORIF. For fresh fractures, surgery was performed at a mean of 3.37 days after injury (range, 0 to 15 d); for delayed fractures, surgery was performed at a mean of 31.67 days after injury (range, 17 to 70 d).
A long arm cast was used for protection immediately after the surgery. The patients were re-evaluated in the clinic 4 weeks postoperatively. If the fracture was healing well and the patient was asymptomatic, the long arm cast was removed. After cast removal, active elbow motion was encouraged. ROM measurements and MEPS evaluation were performed through clinic and telephone follow-up.
Statistical analysis
Categorical and continuous baseline characteristics and perioperative variables are reported as the quantity, percentage, or median and Interquartile Range (IQR), as appropriate. Moreover, continuous variables were compared between two groups by Student’s t test or Mann–Whitney rank sum U tests, while categorical variables were compared by the chi-square test or Fisher’s exact test. After univariable logistic regression, only variables with P<0.1 were submitted to multivariable analysis. A Receiver Operating Characteristic (ROC) curve and the Area Under the ROC Curve (AUC) were used to confirm the predictive ability of the risk factors for lateral spurring. Similar to previous studies, this research used the maximum sum of sensitivity and specificity as the best cut-of value. Relative Risk (RR) was adopted to further assess the influence of the risk factors to the occurrence of lateral spurring.
All tests were 2-tailed, with a P value<0.05 indicating significance. All statistical and graphical analyses were performed using SPSS version 26.0 (IBM SPSS Inc., Chicago, IL, USA).
Results
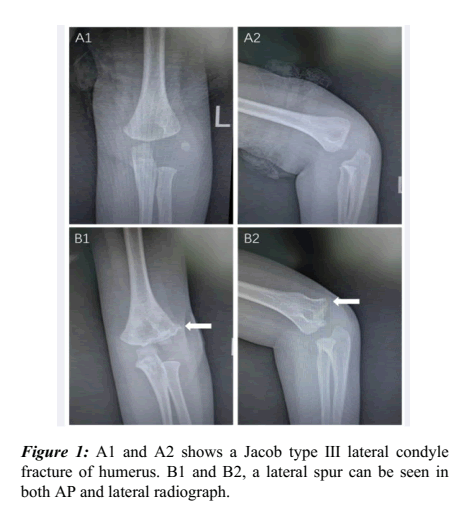
In this retrospectively study, we reviewed the radiographs of 150 pediatric LCFs and found a high incidence of a lateral spur, defined as a bony overgrowth over the lateral of the distal humerus. 4 of the 150 cases are excluded because of insufficient follow-up (<4 w). Therefore, 146 fractures were included in this study. Whether a lateral spur occurred was determined by reading the AP and lateral radiographs approximately half a year (5.19 months average, range, 2-6 months) after the injury (Figure 1).
Clinical characteristics
Of the 146 fractures included in the study, 110 (75.3%) developed a lateral spur, and 36 (24.7%) did not. In Table 1, there were 99 males (67.8%) and 47 females (32.2%) included in the study, with a mean age of 58.50 months (38.75-83.25 m), the clinic and telephone follow-up times were 7.59 months (range, 0-45 months) and 37.87 months (range, 0-91 months), respectively. Of the 146 fractures, 9 (6.2%) were treated with cast immobilization, and 137 (93.8%) were treated with ORIF. Of the 146 fractures, all were Milch type II fractures; 5 were Jacob type I fractures, 44 were Jacob type II fractures, and 97 were Jacob type III fractures. 19 fractures were combined with other elbow injuries (2 with humerus internal condylar fracture, 1 with fracture of proximal radius, 1 with dislocation of elbow joint, and 15 with fracture of proximal ulna). Regarding complications, 7 had cubitus varus (4.8%), 17 had cubitus valgus (11.6%), 1 (0.01%) had nonunion, 4 (2.7%) had incision infection, and 43 (42.2%, only 102 cases had a telephone follow-up) developed a subjective lateral prominence, fishtail deformity or avascular necrosis were not observed. By telephone follow-up, the occurrence of a lateral spur and prominence of humeral lateral condyle did not show a correlation (P=0.731).
| N% | Total (N=146) | Lateral spurring (+) | Lateral spurring (-) | P value |
|---|---|---|---|---|
| Age, monthsa | 58.50 (38.75-83.25) | 51.00 (34.75-72.00) | 89.00 (67.25-106.50) | <0.001 |
| Sex | 0.809 | |||
| Male | 99 | 74 | 25 | |
| Female | 47 | 36 | 11 | |
| BMIa | 17.56 (15.41-19.52) | 17.82 (15.60-19.52) | 17.09 (15.38-19.40) | 0.356 |
| Side of injury | 0.707 | |||
| Right | 65 | 48 | 17 | |
| Left | 81 | 62 | 19 | |
| Jacob type | 0.913 | |||
| Type? | 5 | 2 | 3 | |
| Type? | 44 | 37 | 7 | |
| Type? | 97 | 71 | 26 | |
| Initial displacement | 0.449 | |||
| <2 mm | 27 | 17 | 10 | |
| 2-4 mm | 39 | 33 | 6 | |
| >4 mm | 80 | 60 | 20 | |
| Conservative or surgical | 0.001 | |||
| Conservative | 9 | 7 | 2 | |
| Surgical | 137 | 108 | 29 | |
| ROM loss | <0.001 | |||
| <15° | 134 | 105 | 29 | |
| 15°-30° | 2 | 1 | 1 | |
| 30°-50° | 2 | 0 | 2 | |
| >50° | 2 | 0 | 2 | |
| MEPS | 0.001 | |||
| Excellent | 132 | 104 | 28 | |
| Good | 4 | 3 | 1 | |
| Medium | 3 | 1 | 2 | |
| Poor | 1 | 0 | 1 | |
| Delayed fracture or not | 0.279 | |||
| Yes | 17 | 11 | 6 | |
| No | 129 | 99 | 30 | |
| Combined with other elbow injuries or not | 0.014 | |||
| Yes | 19 | 10 | 9 | |
| No | 127 | 100 | 27 | |
| Complications | ||||
| Cubitus varus | 1 | |||
| Yes | 17 | 13 | 4 | |
| No | 129 | 97 | 32 | |
| Cubitus valgus | 0.487 | |||
| Yes | 7 | 4 | 3 | |
| No | 139 | 106 | 33 | |
| Nonunion | 1 | |||
| Yes | 1 | 1 | 0 | |
| No | 145 | 109 | 36 | |
| Fishtail deformity | 0 | 0 | 0 | |
| Avascular necrosis | 0 | 0 | 0 | |
| Incision infection | 0.567 | |||
| Yes | 4 | 4 | 0 | |
| No | 142 | 106 | 36 | |
| Subjective lateral prominence | 0.731 | |||
| Yes | 43 | 30 | 13 | |
| No | 59 | 43 | 16 |
Table 1: Clinical characteristics of recipients in different prealbumin levels.
Relationship between age and lateral spurring
As shown in Table 2, the clinical characteristics were included in the invariable logistic regression analysis, and the results showed that age, surgical treatment, ROM, MEPS and combined with other elbow injuries were significantly correlated with the incidence of lateral spurring. After multivariable adjustment, age at the time of admission was shown to be an independent predictive factor for lateral spurring. However, given that the amount of fracture displacement is directly correlated with the decision of whether or not to operate, surgical treatment should not be considered as an independent predictor for the development of lateral spurring; age at the time of admission was a protective independent factor for lateral spurring, (OR=0.967; 95%Confidence Interval (CI) 0.952- 0.983; P<0.001).
| Variables | Univariable OR (95% CI) | Univariable P value | Multivariable OR (95% CI) | Multivariable P value |
|---|---|---|---|---|
| Age, months | 0.965 (0.951-0.980) | <0.001 | 0.967?0.952-0.983? | <0.001 |
| Sex | 1.106 (0.490-2.494) | 0.809 | ||
| BMI | 1.077 (0.938-1.237) | 0.292 | ||
| Side of injury | 0.865 (0.407-1.841) | 0.865 | ||
| Jacob type | 0.912 (0.483-1.917) | 0.912 | ||
| Initial displacement | 1.202 (0.747-1.934) | 0.448 | ||
| Conservative or surgical | 13.034 (2.569-66.132) | 0.002 | 10.677?1.453-78.470? | 0.02 |
| ROM | 0.140 (0.021-0.909) | 0.039 | 0.359?0.030-4.240? | 0.416 |
| MEPS | 0.236 (0.075-0.745) | 0.014 | 0.376?0.080-1.782? | 0.218 |
| Delayed fracture or not | 0.556 (0.190-1.628) | 0.284 | ||
| Combined with other elbow injuries or not | 0.300 (0.111-0.812) | 0.018 | 0.934?0.210-4.151? | 0.928 |
| Cubitus varus | 0.415 (0.088-1.950) | 0.265 | ||
| Cubitus valgus | 1.072 (0.321-3.523) | 0.909 | ||
| Subjective lateral prominence | 0.859 (0.361-2.045) | 0.731 |
Table 2: Univariate and multivariate analysis for predictors of postoperative complications.
ROC analysis was used to further investigate the relationship between age and lateral spurring. A cut-off value of 61.5 months calculated by ROC analysis was the optimal criterion, with a sensitivity of 86.1% and specificity of 65.5%, as shown in Figure 2. For predicting lateral spurring after pediatric humerus lateral condyle fractures, the AUC of age was 0.806 (95% (CI) 0.729-0.833; P<0.001). The incidence of a lateral spur was 93.51% (72/77) and 55.07% (38/69) in patients group younger or older than 61.5 months, respectively, the Relative Prevalence (RP) was 1.70.
Discussion
Lateral spurring is the most commonly seen complication after pediatric humerus lateral condyle fractures, with a distinct radiographic deformity. Although this phenomenon has been previously reported, there are still questions remain that unanswered, including its relationship with a deformity in appearance, any possible effects on the overall function of the elbow, and risk factors for its occurrence [2,7,8,11-16].
Previous studies reported the presence of a lateral spur in approximately 70% of pediatric humerus lateral condyle fractures [2,9,13,15]. In our study, 75.3% of the patients subsequently developed a lateral spur, which is similar to the finding previously described by Pribaz et al., [9]. adopted the concept of Interepicondylar Width (IEW), assessed as the maximum distance between the medial and lateral epicondyles of the distal humerus both at the time of admission and at the final follow-up, to describe the severity of a lateral spur. However, we did not use the method because 6.4% (7/110) of the spurs were observed on the lateral radiographs instead of the AP radiograph. Moreover, it was difficult to standardize the appropriate measurement time considering the growth potential of children. Therefore, we did not quantify the severity of a lateral spur.
In our study, age was first found to be a protective independent factor against lateral spurring, the incidence of this complication decreased with age; moreover, patients with age less than 61.5 months were more prone to lateral spurring. This finding can be explained by the overgrowth phenomenon after children’s fractures, which has been observed after fractures of the femur, tibia, and humerus. Bone overgrowth following fracture occurs as a result of hyperemia of fracture healing, and the increased vascularity spreads to the epiphyseal plate leading to growth stimulation and overgrowth. Naik found that remodeling and overgrowth are most pronounced at the growing end of the bone and along the axis of the adjacent joint motion, especially in the case of hinge joints such as the elbow and knee [17-19]. Additionally, an extreme example is, in fractures around the elbow, we found that a bony spur only appeared in pediatric patients. This phenomenon is consistent with Malkawi et al., research: Bony overgrowth was most significant in the 3–9 year age group [20].
Our study once again demonstrated the fact that the presence of a lateral spur has almost no influence on the function of the elbow. Moreover, our study first found that the appearance of the elbow has no correlation with the occurrence of a lateral spur, and subjective lateral prominence seems to be correlated only with the overgrowth of the humerus lateral condyle instead of the spur. These findings will help physicians treating LCFs to reassure patients and families.
This study has several limitations. First, there are inherent limitations with radiographic techniques and results, especially regarding the measurement of the carrying angle. To minimize such limitations, we used standardized techniques performed by an experienced technician and up-to-date digital radiology software, and the patients were also well guided by the technician to obtain the most appropriate position. Additionally, there are no effective methods to quantify the severity of a lateral spur in our study. A lateral spur can be only qualitatively described but not quantitatively measured. In addition, limited by relatively backward treatment concepts, no CRPP was included in our cohort, although other study has proved that there is no significant difference between CRPP and ORIF in the occurrence of a lateral spur [9]. Finally, the current consensus is that LCFs with displacement >2 mm should receive surgical treatment, so surgical treatment still cannot be identified or excluded as an independent risk factor for lateral spurring.
Conclusion
In summary, our study established a database of pediatric patients with LCFs of the humerus to better understand the phenomenon of lateral spurring. As the most common complication after pediatric LCFs, our analysis found that the occurrence of lateral spurring is closely associated the age of patients, and the incidence of this complication decrease with age. Fortunately, the presence of a lateral spur after an LCF of the humerus does not seem to influence the function or appearance of the elbow.
Ethics Approval and Consent to Participate
This study was approved by the ethics committee of the 96603 Military Hospital according to the principles of the Declaration of Helsinki. Written informed consent was waived by the institutional review board for the present study was retrospective.
Consent for Publication
Not applicable.
Availability of Data and Materials
The datasets used and/or analyzed during the current study can be available from the corresponding author on reasonable request.
Competing interests
None declared.
Funding
The present work was unfunded.
Authors’ contributions
Conception: Nan Li. Study design: Nan Li, Tao Liu, Chuan Dong. Data collection and acquisition: Wu Wen. Data analysis: Nan Li, Tao Liu, Chuan Dong. Manuscript preparation: Wu Wen. Figures preparation: Wu Wen. Critical revision: Nan Li. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
References
- Milch H. Fractures and fracture dislocations of the humeral condyles. J Trauma 1964;4(5):592-607.
- Koh KH, Seo SW, Kim KM, et al. Clinical and radiographic results of lateral condylar fracture of distal humerus in children. J Pediatr Orthop 2010;30(5):425-9.
- Park H, Hwang JH, Kwon YU, at al. Osteosynthesis in situ for lateral condyle nonunion in children. J Pediatr Orthop 2015;35(4):334-40.
- Liu TJ, Wang EB, Dai Q, et al. Open reduction and internal fixation for the treatment of fractures of the lateral humeral condyle with an early delayed presentation in children: a radiological and clinical prospective study. Bone Joint J 2016;98(2):244-8.
- Jakob R, Fowles JV, Rang M, et al. Observations concerning fractures of the lateral humeral condyle in children. J Bone Joint Surg Br 1975;57(4):430-6.
- Song KS, Kang CH, Min BW, et al. Closed reduction and internal fixation of displaced unstable lateral condylar fractures of the humerus in children. J Bone Joint Surg Am 2008;90(12):2673-81.
- Badelon O, Bensahel H, Mazda K, et al. Lateral humeral condylar fractures in children: A report of 47 cases. J Pediatr Orthop 1988;8(1):31-4.
- Hasler CC, Von Laer L. Prevention of growth disturbances after fractures of the lateral humeral condyle in children. J Pediatr Orthop B 2001;10(2):123-30.
- Pribaz JR, Bernthal NM, Wong TC, et al. Lateral spurring (overgrowth) after pediatric lateral condyle fractures. J Pediatr Orthop 2012;32(5):456-60.
- Davids JR, Maguire MF, Mubarak SJ, et al. Lateral condylar fracture of the humerus following posttraumatic cubitus varus. J Pediatr Orthop 1994;14(4):466-70.
- Kim DS, Hwang SH, Kwon CS, et al. Results of Treatment of Fracture-Dislocations of Elbow. J Korean Fract Soc Fract 2000 Jan 1;13(1):178-85.
- Bast SC, Hoffer MM, Aval S. Nonoperative treatment for minimally and nondisplaced lateral humeral condyle fractures in children. J Pediatr Orthop 1998;18(4):448-50.
- Conner AN, Smith MG. Displaced fractures of the lateral humeral condyle in children. J Bone Joint Surg Br 1970;52(3):460-4.
- VII C. Elbow fractures in children. Ann Surg 1902;35:75-104. Google Scholar]
[PubMed]
- Launay F, Leet AI, Jacopin S, et al. Lateral humeral condyle fractures in children: a comparison of two approaches to treatment. J Pediatr Orthop 2004;24(4):385-91. [Crossref]
- Thomas DP, Howard AW, Cole WG, et al. Three weeks of Kirschner wire fixation for displaced lateral condylar fractures of the humerus in children. J Pediatr Orthop 2001;21(5):565-9.
- Naik P. Remodelling in children’s fractures and limits of acceptability. Indian J Orthop 2021;55(3):549-59.
- Shapiro F. Fractures of the femoral shaft in children: The overgrowth phenomenon. Acta Orthop Scand 1981;52(6):649-55.
- Emmnaénus H, Hedström Ö. Overgrowth following fracture of humerus in children. Acta Orthop Scand 1965;35(1-4):51-8.
- Malkawi H, Shannak A, Hadidi S. Remodeling after femoral shaft fractures in children treated by the modified blount method. J Pediatr Orthop 1986;6(4):421-9.