Current Pediatric Research
International Journal of Pediatrics
A new procedure for spastic varus/equinovarus foot in children with cerebral palsy: DePuy mitek ® bone micro-absorbable suture anchors.
Song Zhang*, Haibo Zhang, Jie Ma
Department of Pediatric Neurosurgery, Xinhua Hospital, Shanghai JiaoTong University School of Medicine, Shanghai, China
- *Corresponding Author:
- Song Zhang, Department of Pediatric, Neurosurgery Xinhua Hospital, Shanghai JiaoTong University School of Medicine, Shanghai, China, E-mail: zhsg1049@163.com
Received: 03 June, 2022, Manuscript No. AAJCP-22-65427; Editor assigned: 06 June, 2022, PreQC No. AAJCP-22-65427 (PQ); Reviewed: 16 June, 2022, QC No. AAJCP-22-65427; Revised: 22 June, 2022, Manuscript No. AAJCP-22-65427(R); Published: 29 June, 2022, DOI:10.35841/0971-9032.26.6.1454-1457.
We present a new bone micro-absorbable suture anchor technique for spastic varus/equinovarus foot in children with cerebral palsy. Among children, cerebral palsy is the most common serious physical disability. While spasticity is the most common form of hypertonia in Cerebral Palsy (CP) and is experienced by up to 80% of people with CP. Patients with spastic cerebral palsy often have abnormal walking posture due to long-term high muscle tension in the lower limbs, and have pointed feet and varus deformities. A common surgical treatment for spastic varus/equinovarus foot in children with cerebral palsy is tibialis anterior tendon transposition to rebuild ankle dorsiflexion function.
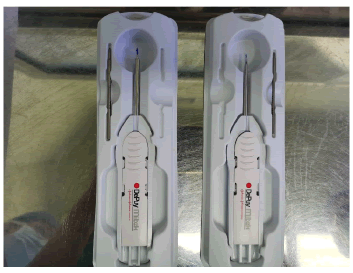
Previously, the transferred tibial anterior tendon was routinely fixed with bone metal suture anchors, which may cause discomfort such as restricted movement after operation, and the long-term indwelling of the anchors in the body, may lead to anchor displacement, slippage, trauma and fracture involving the anchors leading to the risk and complications of anchors removal. Because the sensitivity and mobility of the patient's toes are relatively high, it is required to minimize the damage to the tissues around the tendons and ligaments, and the absorbable suture anchor is the most delicate microabsorbable anchor at present, and it is not easy to cause postoperative complications and discomfort such as restricted movement.
Therefore, we try to use this anchor in clinical practice, and find that the effect is satisfactory, and it also avoided the above-mentioned risks and complications of long-term indwelling of the anchors in the body. Therefore, the bone micro absorbable suture anchor of the spastic varus/equinovarus foot in children with spastic cerebral palsy is an effective technique that does not require hardware removal and is an alternative treatment option to bone metal suture anchors fixation.
Introduction
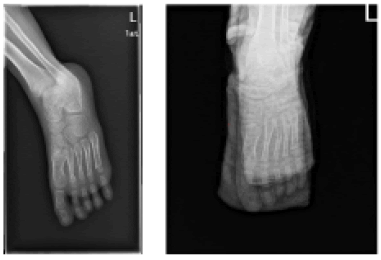
According to the American foot deformity association, the spastic varus foot makes up about 38% of the foot deformities in spastic Cerebral Palsy (CP) unilaterally and 20% in bilaterally. It is mainly due to the imbalance of muscle force distribution, which leads to plantar flexion contracture of the foot, limited dorsiflexion of the ankle joint, adducted and supination deformity of the forefoot, and Achilles tendon contracture,manifested as walking on the lateral edge of the foot or toes on the ground, abnormal gait. The flexible spastic varus foot in cerebral palsy is commonly corrected with splittendon transfers of the tibialis anterior. The goal of this study is to present the DePuy Mitek ® bone micro-absorbable suture anchor, a new technique for spastic varus/equinovarus foot that associates the advantages of surgical fixation with no need for hardware removal. Our hypothesis was that the results of this technique would be similar to those by bone metal suture anchor fixation [1,2].
Materials and Methods
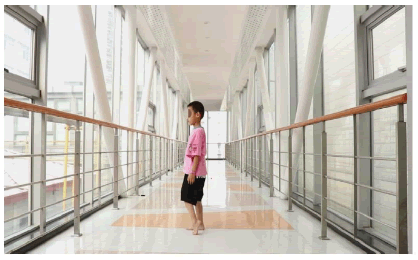
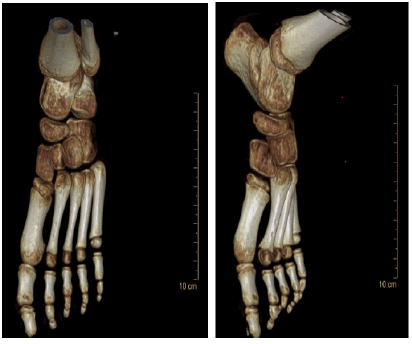
We reviewed a 7 year-old boy with spastic cerebral palsy (Figure 1) who underwent left lower extremity adjustment of muscular strength and tension surgery (CP-MMA) in our hospital in August 2020, using micro-absorbable bone anchors for transposition of the tibialis anterior split-tendon to correct the varus deformity and reconstruct the ankle dorsiflexion function. The follow-up was continued, and the curative effect was satisfactory [3].
Surgical technique
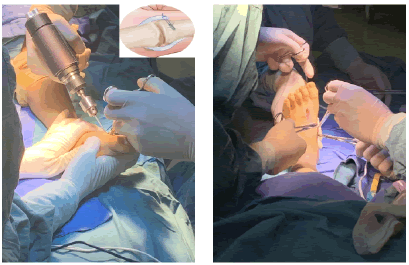
Anesthesia was induced in the patient positioned prone. Under sterile conditions, a lower limb tourniquet was applied on the child's lower leg below the knee. The Achilles tendon was lengthened by 3 cm by percutaneous Achilles tendon elongation, extending the ankle dorsiflexion to 110°. The Tibialis Anterior Tendon (TAT) was exposed through a 4 cm incision in the medial foot where TAT was inserted [4].
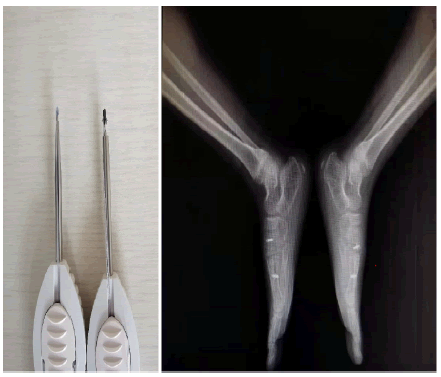
Next, the 75% TAT was cut. And the second metatarsal bone was exposed through a lateral longitudinal skin incision in the dorsum of foot. Two bone micro-absorbable bone anchors were fixed to the hole drilled by electric drill. The TAT was extracted through the subcutaneous tunnel and adapted onto the bone anchors. Finally, the ankle was placed in functional position with a gypsum splint and all incisions were closed (Figure 2) [5].
Results
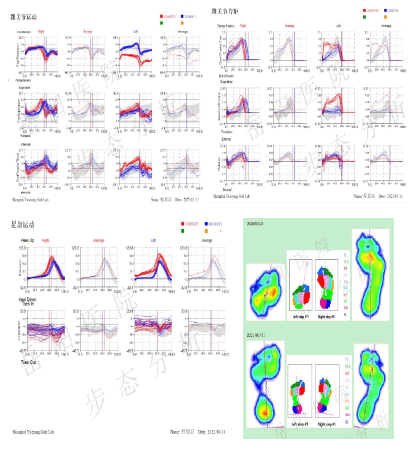
After two weeks, the sutures were removed from the wound, and the family members of the child were informed that they should be immobilized with the plaster splint for at least 6 weeks. He was discharged to a rehabilitation facility in nonweight bearing status. In fact, from the fifth day after the operation until the boy was discharged from the hospital, we asked the rehabilitation therapist to perform bedside training, mainly lower limb strength training and hooking training. Follow-up was conducted five and a half months after the operation, and the changes before and after the operation were compared through three-dimensional gait analysis (Table 1 and Figures 1 to 6), and it was found that the postoperative recovery effect was very satisfactory [6].
| Parameters | Right | Left | ||
|---|---|---|---|---|
| Preoperation | Posoperation | Preoperation | Posoperation | |
| Stretched-Ankle dorsiflexion | 4 | 5 | -7 | 25 |
| Bent-Ankle dorsiflexion | 19 | 20 | -4 | 30 |
Table 1. Comparison of bilateral ankle dorsiflexion angle before and after operation in knee extension and knee flexion
data from Shanghai Yueyang Gait Laboratory.
We did not observe any postoperative complications such as pain or instability. This snail baby (the nickname of the child with cerebral palsy) has almost no abnormality in sports with children of the same age after nearly a year of rehabilitation exercises, and could participate in various activities in physical education classes and outdoor sports [7].
Discussion
This study confirms that bone micro-absorbable suture anchor of the spastic varus/equinovarus foot in children with cerebral palsy are a reliable technique and that the result are equivalent to those of the reference metal suture anchors fixation technique. The strong points of our study are the original technique [8].
The limits to our study were the retrospective observations and early attempts and the small size of the study population (We have done a total of 6 children with cerebral palsy with varus feet, a total of 8 spastic feet with micro-absorbable bone anchors, and the remaining cases are still under follow-up) [9].
Up to now, through our follow-up, the child has not experienced any discomfort or complications after surgery. Previously, the transferred tibial anterior tendon was routinely fixed with bone metal suture anchors (Figure 7), which may cause discomfort such as restricted movement after operation, and the long-term indwelling of the anchors in the body, may lead to anchor displacement, slippage, trauma and fracture involving the anchors leading to the risk and complications of anchors removal [10,11].
Conclusion
Bone micro-absorbable suture anchors are a feasible technique in clinical practice with results that are equivalent to those of conventional techniques. It is not worried about the risk of complications of taking the anchor in the future, because the body is made of the absorbable material polylactic acid. This is an obvious advantage for cost and morbidity. Learning the surgical technique requires a learning curve, and it must be rigorously applied.
Disclosure of interest
There are no competing interests between the authors.
References
- Bennet GC, Rang M, Jones Paterson D. Varus and valgus deformities of the foot in cerebral palsy. J Dev Med Child Neurol 2008, 50: 164.
[Crossref] [Google Scholar] [Indexed]
- Dussa CU, Böhm H, Döderlein L, et al. Treatment of spastic varus/equinovarus foot with split-tendon transfers in cerebral palsy: How does it affect the hind foot motion? J Gait Posture 2022; 92: 343-50.
[Crossref] [Google Scholar] [Indexed]
- Cheng-Li L, Chii-Jeng L, Ming-Tung H, et al. Mesh Achilles tendon lengthening a new method to treat equines deformity in patients with spastic cerebral palsy: Surgical technique and early results. J Pediatr Orthop B 2013; 22: 14-9.
[Crossref] [Google Scholar] [Indexed]
- Brustein M, Pellegrini J, Choueka J, et al. Bone suture anchors versus the pullout button for repair of distal profundus tendon injuries: A comparison of strength in human cadaveric hands. J Hand Surg Am 2001; 26: 489-96.
[Crossref] [Google Scholar] [Indexed]
- Chul-Hyun C, Ki-Cheor B, Du-Han K. Biomaterials Used for Suture Anchors in Orthopedic Surgery. Clin Orthop Surg 2021; 13: 287-292.
[Crossref] [Google Scholar] [Indexed]
- Yangjing L, Cao J, Changgui Z, et al. Modified Percutaneous Achilles Tendon Lengthening by Triple Hemisection for Achilles Tendon Contracture. Biomed Res Int 2019; 1491796.
[Crossref] [Google Scholar] [Indexed]
- https://europepmc.org/article/med/8416348
- Hoffer MM, Reiswig JA, Garrett AM, et al. The split anteriortibial tendon transfer in the treatment of spastic varus hindfoot of childhood. Orthop Clin North Am 1974; 31–38.
- Liggio FJ, Kruse R. Split tibialis posterior tendon transfer with concomitant distal tibial derotational osteotomy in children with cerebral palsy. J Pediatr Orthop 2001; 21(1) 95–101.
[Crossref] [Google Scholar] [Indexed]
- https://online.boneandjoint.org.uk/doi/abs/10.1302/1358-992X.94BSUPP_XXXVII.EFORT2011-146
- Kläusler M, Speth Bernhard M, Brunner R, et al. Long-term follow-up after tibialis anterior tendon shortening in combination with Achilles tendon lengthening in spastic equinus in cerebral palsy. Gait Posture 2017; 58: 457-462.
[Crossref] [Google Scholar] [Indexed]