Current Pediatric Research
International Journal of Pediatrics
A case of short stature found to be Laron Syndrome: A case report
Pediatric Department, King Abdulaziz University, Jeddah, Saudi Arabia
- Corresponding Author:
- Abdulmoein Eid Al-Agha
Professor, Department of Pediatric Endocrinology, Pediatric Department
King Abdulaziz University Hospital PO Box-80215, Jeddah 21589, Saudi Arabia
Fax: +966 2 640 3841
Tel: +966 2 6408353
E-mail: aagha@kau.edu.sa
Accepted date: August 28th, 2018
Laron syndrome is a rare cause of short stature due to an autosomal recessive disorder that results in growth hormone resistance, with an estimation of 300 cases worldwide. We report the case of a 10-year-old female patient who was presented with severe short stature and found to have growth hormone resistance, and was finally diagnosed with Laron syndrome.
Keywords
Laron, Syndrome, Short stature, Growth hormone, Receptor resistance.
Introduction
Laron Syndrome (LS) is an autosomal recessive disorder that causes short stature due to growth hormone insensitivity, despite the high levels of growth hormone [1-3]. Since its first report in 1966, more than 250 cases has been reported worldwide [3,4]. LS is found among Mediterranean, Middle Eastern, or South Asian families who tend to form marital relations among relatives or practice consanguinity [3,4].
The molecular mechanism of LS can be attributable to mutation of growth hormone receptor gene. In cases of LS, receptor polymorphism results in the inability to generate Insulin-Like Growth Factor 1 (IGF-1) [2,3]. In this syndrome, IGF-1 and IGF-BP3 are markedly low despite normal or elevated serum levels of growth hormone, as there is an unresponsiveness to endogenous and exogenous GH [4]. Mutations in the single gene responsible for GH receptor synthesis can disrupt the nature of the extracellular binding domain of the receptor, preventing the hormone from binding, and result in LS [4-6]. Many mutations has been identified in the growth hormone receptor gene (insertions, deletions missense, non-sense, or abnormal splicing) [1,3]. The receptor has an extracellular growth hormone binding domain, and mutations in this extracellular domain interfere with binding of growth hormone, resulting in LS [3]. Only a few mutations has been reported to be affecting the transmembrane or intracellular domains [4].
Short stature is the main and most impelling effect of LS; other symptoms include reduced muscle strength, hypoglycemia, small genitals among males, delayed puberty, and dental abnormalities [4]. The individuals with LS show the characteristic features such as protruded forehead, saddle nose, blue sclera, and small hands and feet. They have poor prognosis due to the difficulty in treatment [4].
Left untreated, the height of patients with LS is a chronic problem. Some of them progressively develop hyperinsulinemia followed by hypoinsulinemia, glucose intolerance and, around puberty, even diabetes and obesity with hyperlipidemia [2]. We report the case of a 10-yearold female patient who was presented with severe short stature and found to have growth hormone resistance, and was finally diagnosed with Laron syndrome.
Case Report
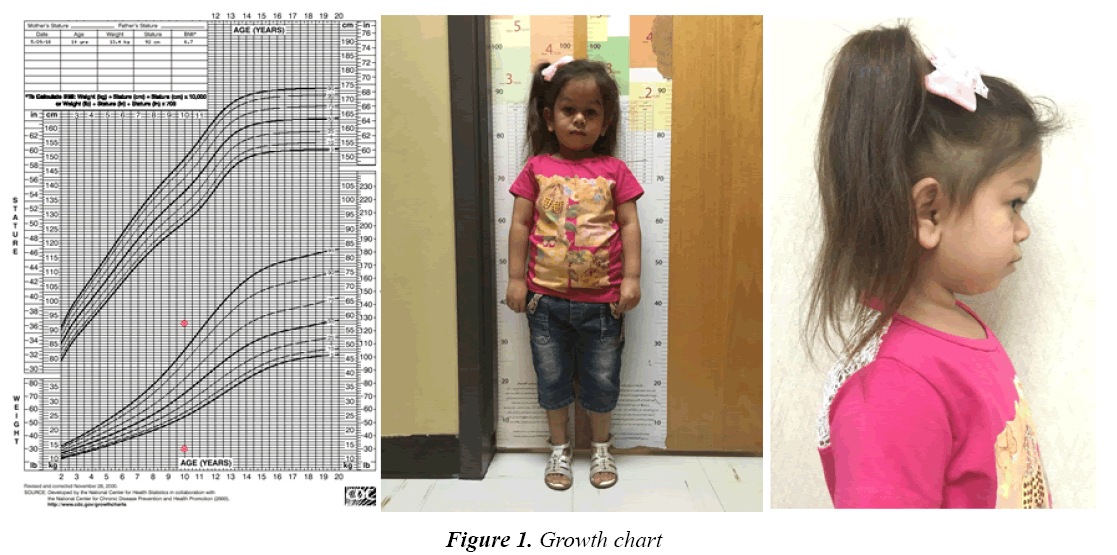
A 10-Year-old Saudi girl presented to our endocrinology clinic with no history of medial illness. She was a product of spontaneous vaginal delivery after an uneventful pregnancy at full term, with no birth complications such as birth asphyxia. She had a weight of 3.2 kg and height of 47 cm at birth. Upon presentation to the clinic, she was noted to be short at a height of 92 cm (standard deviation -7.8), and had a weight of 13.4 kg (standard deviation -6.3), a head circumference of 49 cm, and body mass index of 15 (40th percentile). Her upper to lower segment ratio was 1.15:1. She was reported to have reached her developmental milestones at the appropriate ages, had an episode of hypoglycemia as a child, and has two brothers who are short. The parents are cousins and had no past history of short stature in the family. Upon examination she was noted to have protruded forehead, thin hair, small hands and feet, and a saddle nose. No teething defects were found, and no blue sclera was observed (Figure 1).
She was subjected to the following further investigations (Table 1): growth hormone stimulation test was done using the double agents glucagon and levodopa, as the constant high levels of growth hormone raised the suspicion of GH insensitivity. Table 2 shows the results of GHF-1 generation test, in which the baseline IGF-1 level was obtained first, then a dose of 60 mg somatotropin was given subcutaneously at the same time of the day (preferably at bedtime) for 4 days. On the fifth day the IGF-1 was measured again. A normal individual will show an increase in IGF-1 levels, and in cases of GH resistance no increase would be found [3,7].
| Parameter | Value | Reference Range |
|---|---|---|
| Growth Hormone (Stimulation Test) | ||
| Basal (0 min) | 28.48 ng/mL | Up to 10 ng/mL |
| Give Levadopa | ||
| 30 min | 28.86 ng/mL | Up to 10 ng/mL |
| 60 min | 40.13 ng/mL | Up to 10 ng/mL |
| Give Glucagon | ||
| 90 min | 27.22 ng/mL | Up to 10 ng/mL |
| 120 min | 27.64 ng/mL | Up to 10 ng/mL |
| 150 min | 21.76 ng/mL | Up to 10 ng/mL |
| 180 min | 17.18 ng/mL | Up to 10 ng/mL |
| 210 min | 11.62 ng/mL | Up to 10 ng/mL |
Table 1: Growth hormone stimulation test
| IGF-1 Generation test | ||
| IGF-1 on [13/2/18] | 25.0 ng/mL | |
| 4 days of [60 mg] Somatotropin | ||
| IGF-1 on [18/2/18] | 25.0 ng/mL | |
Table 2: IGF-1 Generation test
The final diagnosis was confirmed, as the patient had high levels of GH and no response to IGF-1 stimulation test, this was concluded as GH insensitivity syndrome Known as Laron Syndrome, and the treatment using recombinant insulin like growth hormone factor 1 was indicated.
Discussion
Short stature is defined as a height below 3rd percentile, lower than the normal average by 2 or more standard deviations. It is sometimes classified as either proportional short stature or dysproportional short stature such as cases of achodroplasia, hypochondroplasia and multiple epiphyseal dysplasia [8,9]. It can be further classified according to etiology as nutritional, gastrointestinal, and endocrine [7]. Endocrine causes of short stature include hormone deficiencies such as GH deficiency, of which LS is a subtype [8, 9]. An estimation of 300 patients have LS worldwide, and many of them belong to consanguineous families.
Extreme short stature with more than 4 SD below the mean is usually the most prominent clinical presentation, as seen in our patient. In LS patients, birth weight and height are normally within normal range at birth [4,5]. Protruding forehead, saddle nose, small hands and feet (acromilia) and short limbs with upper segment: lower segment ratio more than 1, which are typical features of Laron syndrome were seen in our patient [4-6].
Those patients could present with severe hypoglycemia in early childhood, caused by low glucose output from the liver in the absence of IGF-1 [4,5], this has been noticed on our patient but no diagnosis approach was taken at that time.
Other features of LS include delayed fontanel closure, shallow orbits, and the setting sun sign of the eyes. Blue sclera may be noted, particularly in patients of Mediterranean or Middle Eastern origin [4]. Hair growth is quite sparse in infancy and through early childhood. It is silky and forms temporal and frontal recessions [4,6].
Another condition that could present in a similar picture is GH-gene deletion syndrome [10], which is caused by many identified mutations. GH-gene deletion syndrome can present with the same appearance of acromicria, organomicria, retarded development of the skeletal and muscular systems, cranio-facial disproportion and obesity [11,12]. Both LS and GH-gene deletion syndrome have undetectable levels of circulating IGF-1, but GH levels are very high in the sera of patients with LS due to an insensitivity of GH-receptors, while they are undetectable in those with GH-gene deletion [12].
The prognosis of LS is considered unfavorable without treatment. Untreated male patients reach a final height of 116 to 142 cm, and females reach a height of 108 to 136 cm. Laron dwarfism courses with hip dysplasia (commonly), dental, eye and hearing problems [4].
In our case, we noted short stature in the patient, with normal levels of GH. GH stimulation test suggested resistence to GH. The confirmation was done using IGF-1 generation test. Treatment of LS consists of recombinant IGF-I improves growth rate initially, starting as early as possible and continue through life, yet these patient does not seem to be able to reach normal height [13,14]. Intermittent therapy is shown to be equally cost effective as daily treatment [4,15].
Evidence exists that rIGF-1 therapy also reduces body fat, stimulates kidney function, and maintains left ventricle dimension and function within the normal range of agematched control subjects [3,4].
Conclusion
In conclusion this is a presentation of a special case of short stature, in which the approach to such cases was discussed, LS is a rare disease and many cases need to be reported in order to reach better understanding of the disease.
References
- Sugunakar C, Rao NN, Sarma MBR. A rare presentation of clinical short stature due to insensitivity of growth hormone (Loran syndrome). J Evolution Med Dent Sci 2013; 2: 10032-10036.
- Castilla‐Cortazar I, Femat‐Roldán G, Rodríguez‐Rivera J, et al. Mexican case report of a never‐treated Laron syndrome patient evolving to metabolic syndrome, type 2 diabetes, and stroke. Clin Case Rep 2017; 5: 1852-1855.
- Cotta OR, Santarpia L, Curto L, et al. Primary growth hormone insensitivity (Laron syndrome) and acquired hypothyroidism: a case report. J Med Case Rep 2011; 5: 301.
- Laron Z. Lessons from 50 years of study of Laron syndrome. End Pract 2015; 21: 1395-1402.
- Moia S, Tessaris D, Einaudi S, et al. Compound heterozygosity for two GHR missense mutations in a patient affected by Laron Syndrome: a case report. Ital J Pediatr 2017; 43: 94.
- Lurie R, Ben-Amitai D, Laron Z. Laron syndrome (primary growth hormone insensitivity): a unique model to explore the effect of insulin-like growth factor 1 deficiency on human hair. Dermatology 2004; 208: 314-318.
- Yadav S, Dabas A. Approach to short stature. Indian J Pediatr 2015; 82: 462-470.
- Hasegawa K, Tanaka H. Children with short‐limbed short stature in pediatric endocrinological services in Japan. Pediatr Intern 2014; 56; 809-812.
- Saengkaew T, McNeil E, Jaruratanasirikul S. Etiologies of short stature in a pediatric endocrine clinic in Southern Thailand. J Pediatr End Met 2017; 30: 1265-1270.
- Ogawa M, Kamijo T, Igarashi Y, et al. Prevalence of GH-1 Gene Deletion in Patients with Isolated Growth Hormone Deficiency in Japan. End J 2000; 47: 157-162.
- Laron Z, Ginsberg S, Webb M. Nonalcoholic fatty liver in patients with Laron syndrome and GH gene deletion–preliminary report. Growth Horm IGF Res 2008; 18: 434-438.
- Ahmad T, Geffner M, Parks J, et al. Short stature and metabolic abnormalities in two sisters with a 7.6-kb GH1 gene deletion. Growth Horm IGF Res 2011; 21: 37-43.
- Messina MF, De Luca F, Wasniewska M, et al. Final height in isolated GH deficiency type 1A: effects of 5-year treatment with IGF-I. Eur J Endocrinol 2001; 144: 379-383.
- Messina MF, Arrigo T, Valenzise M, et al. Long-term auxological and pubertal outcome of patients with hereditary insulin-like growth factor-I deficiency (Laron and growth hormone-gene deletion syndrome) treated with recombinant human insulin-like growth factor-I. J Endocrinol Invest 2011; 34: 292-295.
- Latrech H, Simon A, Beltrand J, et al. Postprandial hyperglycemia corrected by IGF-I (Increlex®) in Laron syndrome. Horm Res Paediatr 2012; 78: 193-200.